Anthracofibrosis is a bronchial stenosis due to local mucosal fibrosis that also presents anthracotic pigment in the mucosa. The cause has not been well clarified, although there is a frequent association with tuberculosis and the exposure to smoke from biofuel or biomass combustion. It is an entity that has not been reported in Spain, although the influx of people from rural areas of developing countries or rural areas of our own country should make us contemplate this entity in the differential diagnosis of our patients.
We present 3 cases detected in Spain (2 of them natives) diagnosed by bronchoscopy and bronchial biopsy, which are techniques necessary to confirm the diagnosis. There is no specific treatment, except for tuberculostatic treatment in cases with coexisting tuberculosis.
La antracofibrosis es una estenosis bronquial debida a una fibrosis mucosa local que presenta además una mucosa con pigmento antracótico. La causa no está bien aclarada, y se da una frecuente asociación con la tuberculosis y la exposición a humos de combustión de biocombustibles (o biomasa). Se trata de una entidad no descrita en España, aunque la afluencia de personas originarias de zonas rurales de países en desarrollo o de zonas rurales de nuestro medio debe hacernos tener presente esta entidad en el diagnóstico diferencial de nuestros pacientes.
Se presentan 3 casos detectados en España (2 de ellos autóctonos) diagnosticados mediante broncoscopia y biopsia bronquial, técnicas necesarias para su confirmación. No hay tratamiento específico, salvo el tuberculostático en el caso de coexistencia de ambas entidades.
Anthracofibrosis, also known as anthracostenosis or bronchial anthracosis, is its own entity and is different from coal worker's pneumoconiosis. It is defined as a bronchial stenosis, which may vary in degree (Fig. 1) and is due to a local mucous fibrosis that also presents mucosa with anthracotic pigment1–3 (Fig. 2). Initially described by Abraham4 in 1951, it was not until 1998 that Chung5 coined the term “anthracofibrosis”. On occasions, there may be findings of distal (bronchiolar) anthracosis, but the vast majority is located at the bronchial level and is therefore described as a different entity in both its presentation as well as its causal hypotheses. This entity is more frequent in older non-smoker women from rural areas of Asia (especially the Middle East and Far East). Anthracofibrosis was not reported in Europeans until 2008 (in England), and no cases have been reported in Spain until now. It has an important relationship with pulmonary tuberculosis,6,7 an entity that is present in 30%–60%8 of the cases, which has been postulated as one of the possible causes. In other cases, anthracofibrosis is associated with the inhalation of biomass fuel smoke, especially animal manure. Radiologically, local thickening of the bronchial mucosa is usually observed, which frequently leads to stenosis, causing distal atelectasis (Fig. 1). Furthermore, it is usually accompanied by local lymphadenopathies. It commonly affects the lobar or segmental bronchi in varying numbers (more frequently between 1 and 5 segments), and does not affect the trachea or main bronchi.8
We present below 3 patients with anthracofibrosis that have been detected in our country.
Clinical NotesCase 1A 74-year-old Indian woman who has been living in the Spanish Balearic Islands for the last three years, with no toxic habits or medical history of interest. She was studied due to dysphagia to solids which had been evolving over a long period of time, with no other symptoms. On thoracic CT, a mass of atelectasis in the left upper lobe and calcified hilar lymphadenopathies were observed. Bronchoscopy showed a multitude of disperse black maculae in the bilateral bronchial mucosa with stenosis at the culmen of the left upper lobe due to a very friable blackish-purple nodule. The histology showed fibrosis of the mucosa accompanied by anthracite deposit with no granulomas or atypia. The Ziehl-Neelsen stain was negative, and the Löwenstein culture was positive for Mycobacterium tuberculosis growth. Tuberculostatic treatment was established, with no radiological improvement. When we questioned the patient, she denied any occupational exposure to biomass combustion (she was employed as domestic help) although during her childhood she lived in a rural area where the combustion of biomass was commonly used in homes.
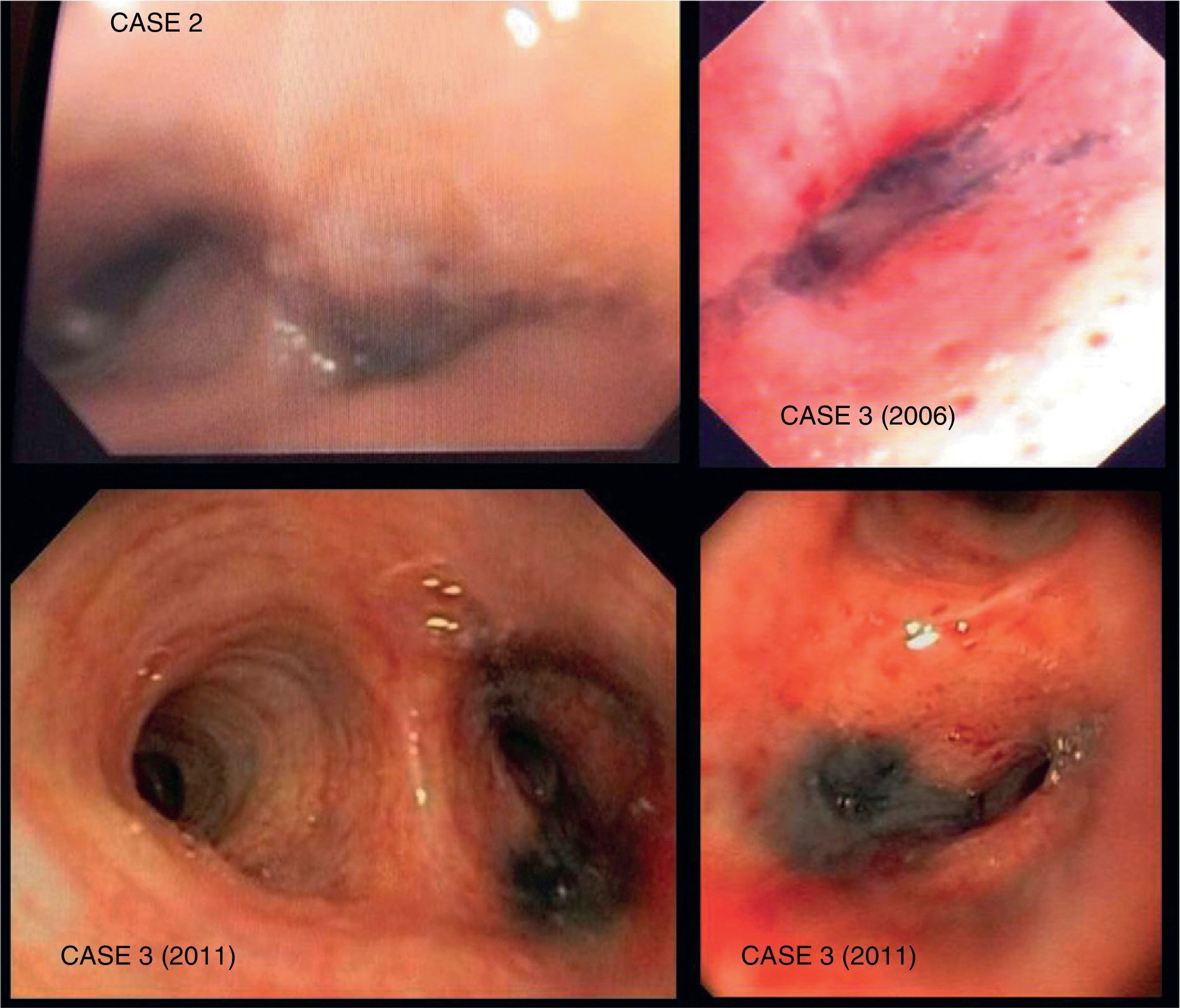
Case 2An 88-year-old male from the Spanish Balearic Islands, with no toxic habits, who had worked as a silversmith using coal to melt down silver. He was admitted for pneumococcal pneumonia in the left lower lobe. Treated with levofloxacin, he showed a clear clinical improvement, but there was partial atelectasis in the left lower lobe. Thoracic CT demonstrated a mass/infiltrate with total atelectasis of the left segment 6 and partial atelectasis of the left lower lobe and the lingula. Bronchoscopy (Fig. 2) showed millimetric blackish-purple maculae that were anthracotic in appearance in the bilateral segmental and lobar bronchi, with subtotal stenosis of the lumen of the left lower lobe due to blackish-purple nodules. Histology revealed chronic acute inflammation with local fibrosis and anthracotic deposit, with no evidence of malignancy or pathogens. Bronchoscopy was repeated 2 months later, with the same results. Tuberculosis bacilli were not isolated, and therefore specific treatment was not started.
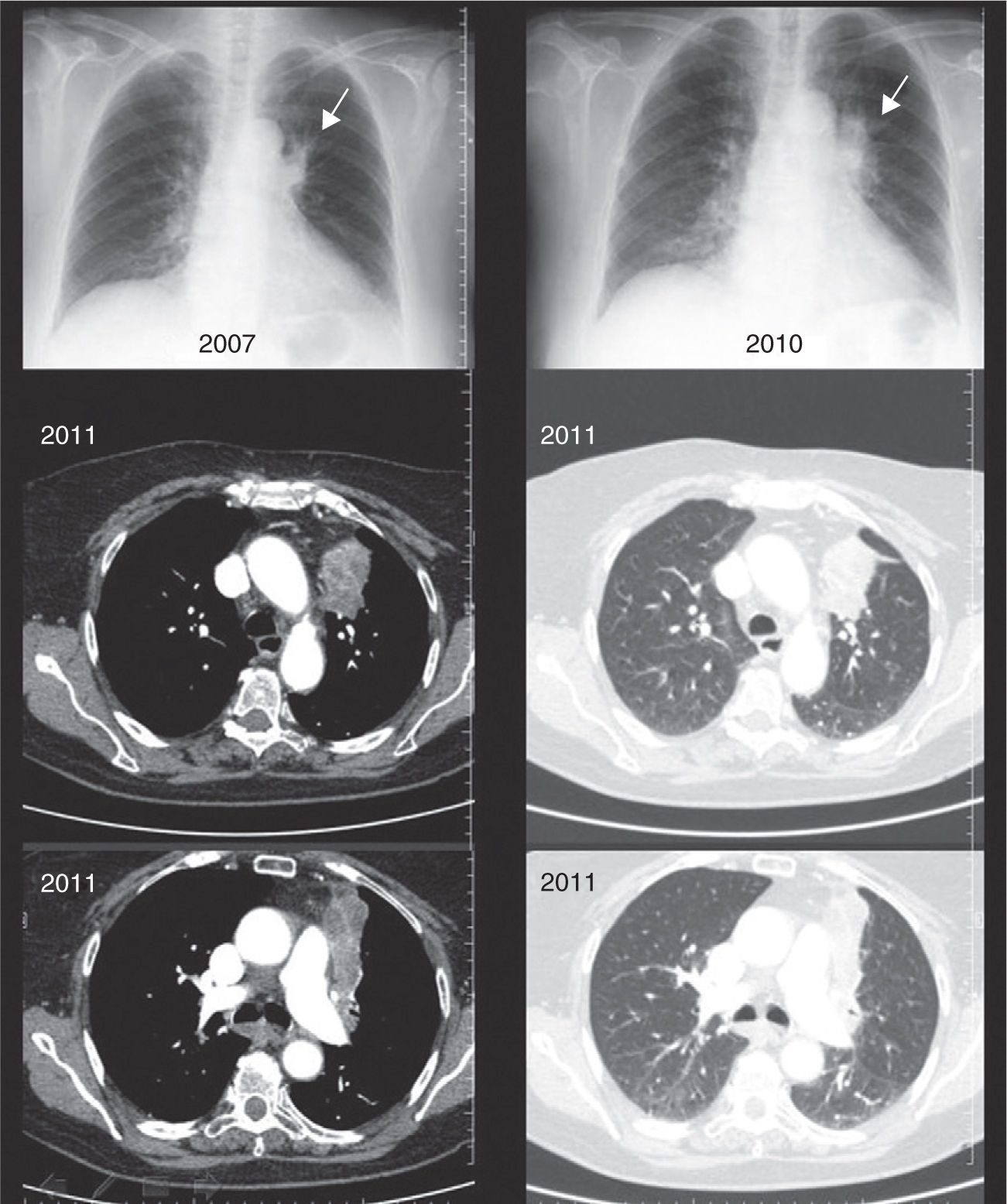
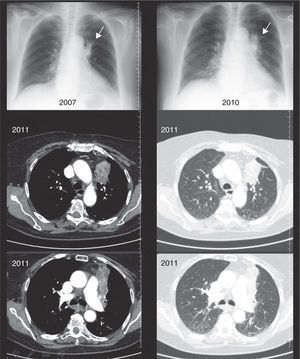
Case 3An 84-year-old woman from Madrid with no toxic habits who, during her childhood and youth (from 0 to 25 years of age) was regularly exposed to the domestic use of kerosene and coal stoves. She later worked in domestic service, with no later exposure to biomass. In 2006, she underwent studies due to triangular infiltrates in the anterior area of the left upper lobe (Fig. 1) confirmed by slow-resolution chest CT. Afterwards, 2 bronchoscopies showed edema and stenosis of the opening of the culmen segments of the left upper lobe with blackish-purple mucosa (Fig. 2), together with the growth of enterobacteriaceae and Haemophilus influenzae on respective endoscopies. The patient was treated as determined by the antibiogram, and there was a small radiological improvement; there is no later follow-up or data on the patient's evolution. The histology of the biopsies showed no evidence of malignancy, and there was no diagnostic conclusion. In 2010, the patient was again remitted for study of infiltrates in the anterior segment of the left upper lobe (Fig. 1), which did not improve after a cycle of Cefditoren. A new CT showed a heterogeneous mass/atelectasis in the anterior segment of the left upper lobe that encompassed the segmental bronchus, causing it to be obstructed, with loss of volume of the left upper lobe (Fig. 2). In addition, a 1-cm right paratracheal lymphadenopathy was observed. Given the suspicion for neoplasm, another bronchoscopy was performed (Fig. 2), which showed a black vegetative mass that stenosed the anterior and apical-posterior opening of the left upper lobe. Upon biopsy, the tissue showed mucosa with fibrous chorion and abundant anthracosis with no data for malignancy. The cultures were negative. Tuberculosis bacilli were not isolated, and therefore specific treatment was not started.
DiscussionAnthracofibrosis is an entity that has not been reported in our setting. It is characterized by black pigmentation of the bronchial mucosa due to anthracotic deposits9 together with local inflammation and finally fibrosis that distort and stenose said bronchus (Fig. 2) with potential atelectasis of the tributary parenchyma (Fig. 1). The cause of said entity has not been completely clarified, although various hypotheses have been postulated. First is the tuberculosis hypothesis,6,7 explained by the tuberculous reactivation of lymphadenopathies adjacent to the bronchus that infiltrate and continuously fistulize the wall of the bronchus with caseous granulomatous inflammation and later local fibrosis.4 Anthracotic pigmentation is supposedly due to the fact that the lymph nodes of people exposed to smoke or coal have anthracite particles responsible for the coloration as they are in contact with the bronchial wall. This hypothesis would explain the highly frequent (30%–60%)8 association of anthracofibrosis and tuberculosis, as in the first case described. Different publications are also in favor of this hypothesis, reporting partial radiological improvement after tuberculostatic treatment,5,7 although there is no evidence of resolution with said treatment.
Nevertheless, it is not completely clear that this may be the only possible cause, because it would not explain why there is negativity for tuberculosis in 40%–70% of the remaining cases, in spite of repeat cultures. This is why another hypothesis is being contemplated which would explain why the pathogenic mechanism would be the exposure to the incomplete combustion smoke of biomass fuels10 in places with limited ventilation. Approximately half of the world's population, and up to 90% of homes11,12 in rural areas of developing countries, still depend on the combustion of biomass fuels (wood, manure and harvest residues) for cooking and heating, which produces incomplete combustion and generates inhalable particles, carbon monoxide, nitrogen oxide, organic hydrocarbons and other toxic compositions. In developing countries, it is traditionally women13 who are responsible for the cooking, and are therefore more exposed, as are the children in their care, which explains the high prevalence in elderly women from rural areas in developing countries with no tobacco habit.14,15 In Spain, it is not infrequent to find the use of coal or wood-burning stoves that heat the parts of the houses where families spend most of their time. This is true mostly in rural areas with colder climates, as occurred in the third case we have described. The second case has similar causal hypothesis, but due to occupational exposure to coal combustion. It is striking that it is exactly in the patients who do not declare contact with the combustion of biomass fuels where it seems that more cases of tuberculosis are detected and, therefore, a greater frequency of granulomas are observed on histology.7 Meanwhile, in patients exposed to biomass combustion, less cases of tuberculosis are isolated, and therefore in said cases no response is observed to empirical tuberculosis treatment.5,16 Thus, it is more than likely that we are faced with two possible causes of one same entity in which, due to one mechanism or another, there is a resulting endobronquial deposit of anthracite with an inflammatory response that leads to local fibrosis. According to the inhalation hypothesis, the difference between coal miner's pneumoconiosis17 and anthracofibrosis could be explained by the differing sizes of the inhaled particles, which would favor reaching the distal airway in the former (coal dust without combustion, 1–2μm), while in anthracofibrosis these would be larger in caliber (5–10μm, volatilized in combustion smoke) and become trapped more proximally.18 In addition, it must be kept in mind that, in the case of anthracofibrosis, said particles would be higher in temperature, which could favor greater local inflammation. Regarding the substances involved in the pathogeny of anthracofibrosis, electron microscope studies of the bronchoalveolar lavage of affected patients have detected, in addition to coal, other substances such as silica, mica, kaolinite and other silicates.19,20
Finally, there could be a mixed causal hypothesis somewhere between the tuberculosis and inhalation hypotheses. This would advocate the exposure to biomass combustion smoke being responsible for reduced mucociliary clearance and reduced activity of the alveolar macrophages as well as the cellular immune response,18 all of which would favor the greater presence of cases of tuberculosis in these persons and the frequent coexistence of both entities.
Thus, in conclusion, this nosological entity should be kept in mind when faced with persistent atelectasis as an alternative diagnosis to lung cancer8 in patients from areas with greater exposure to biomass combustion, especially in older women with no previous tobacco history.14,15 The frequent association with tuberculosis should also be considered and studies should be performed aimed at either ruling out or confirming said association in each specific case, as well as its treatment in cases with microbiological confirmation.
Conflict of InterestsThe authors declare having no conflict of interests.
The authors would like express their gratitude towards Ms. Raquel Sanz Izquierdo, RN at the Hospital Mateu Orfila in Menorca, who died in South Africa on 17 October 2010, and acknowledge her constant example of love, dedication and devotion that she always showed for her patients.
Please cite this article as: Gómez-Seco J, et al. Antracofibrosis o antracoestenosis. Arch Bronconeumol. 2012;48:133-6.