Historically, the epidemiological burden of tuberculosis (TB) has been larger in men than in women and, in many societies, exposure to infectious cases differs between both sexes.1 Every year, more cases of TB are documented in men than in women worldwide,2 and prevailing surveys show this disparity.3
The study's goals were: to identify the characteristics and risk factors associated with gender and tuberculosis (TB), assess the linear trend of the incidence of cases by over time, and determine whether there are differences in diagnostic delay and treatment compliance.
All TB cases included in the Integrated Programme of Research in Tuberculosis and Non-Tuberculosis Mycobacteria (PII-TB&MNT) of SEPAR between 2017 and 2022 were included in a cross-central multicenter study. The χ2 test was used to analyze the gender differences, considering that they were statistically significant if p-value <0,05. A binary logistic regression was used and odds ratios (OR) and 95% confidence intervals (CI) were computed. The temporal trend of the variable was obtained using the χ2 linear trend test. IBM SPSS Statistics 22 statistical software was used to conduct the analysis.
The processing of personal data was in accordance with Spanish Organic Law 3/2018, of 5 December, on the Protection of Personal Data and the Guarantee of Digital Rights and the European Data Privacy Directive.
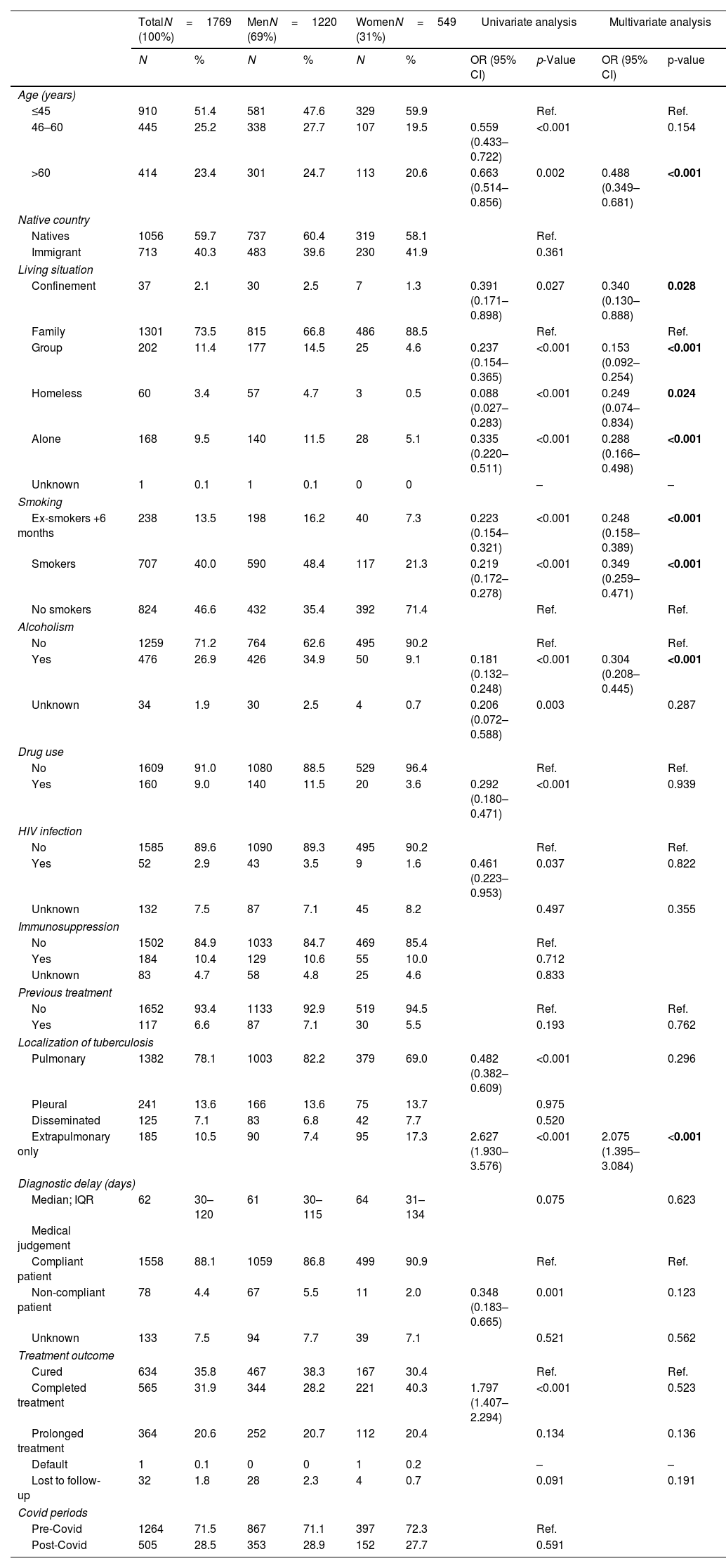
A sample of 1769 cases included in the registration between 2017 and 2020 was studied, of which 1220 (69%) were men and 549 women (31%). Multivariate analysis showed significant gender differences associated with men in the following categories: aged >60; in confinement; living alone or in groups; homeless; consume tobacco or alcohol. However, extrapulmonary localization was more common in women. There were no differences in the rates of diagnostic delay. There were no differences in the rates of diagnostic delay. There were differences in treatment compliance and treatment outcome, but these were not statistically significant (Table 1). There were also no significant differences in the pre-Covid and post-Covid periods in the ratio of men and women (p=0.59).
Sociodemographic, Epidemiological, Clinical, Diagnostic and Treatment Characteristics and Risk Factors by Gender.
| TotalN=1769 (100%) | MenN=1220 (69%) | WomenN=549 (31%) | Univariate analysis | Multivariate analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | OR (95% CI) | p-Value | OR (95% CI) | p-value | |
| Age (years) | ||||||||||
| ≤45 | 910 | 51.4 | 581 | 47.6 | 329 | 59.9 | Ref. | Ref. | ||
| 46–60 | 445 | 25.2 | 338 | 27.7 | 107 | 19.5 | 0.559 (0.433–0.722) | <0.001 | 0.154 | |
| >60 | 414 | 23.4 | 301 | 24.7 | 113 | 20.6 | 0.663 (0.514–0.856) | 0.002 | 0.488 (0.349–0.681) | <0.001 |
| Native country | ||||||||||
| Natives | 1056 | 59.7 | 737 | 60.4 | 319 | 58.1 | Ref. | |||
| Immigrant | 713 | 40.3 | 483 | 39.6 | 230 | 41.9 | 0.361 | |||
| Living situation | ||||||||||
| Confinement | 37 | 2.1 | 30 | 2.5 | 7 | 1.3 | 0.391 (0.171–0.898) | 0.027 | 0.340 (0.130–0.888) | 0.028 |
| Family | 1301 | 73.5 | 815 | 66.8 | 486 | 88.5 | Ref. | Ref. | ||
| Group | 202 | 11.4 | 177 | 14.5 | 25 | 4.6 | 0.237 (0.154–0.365) | <0.001 | 0.153 (0.092–0.254) | <0.001 |
| Homeless | 60 | 3.4 | 57 | 4.7 | 3 | 0.5 | 0.088 (0.027–0.283) | <0.001 | 0.249 (0.074–0.834) | 0.024 |
| Alone | 168 | 9.5 | 140 | 11.5 | 28 | 5.1 | 0.335 (0.220–0.511) | <0.001 | 0.288 (0.166–0.498) | <0.001 |
| Unknown | 1 | 0.1 | 1 | 0.1 | 0 | 0 | – | – | ||
| Smoking | ||||||||||
| Ex-smokers +6 months | 238 | 13.5 | 198 | 16.2 | 40 | 7.3 | 0.223 (0.154–0.321) | <0.001 | 0.248 (0.158–0.389) | <0.001 |
| Smokers | 707 | 40.0 | 590 | 48.4 | 117 | 21.3 | 0.219 (0.172–0.278) | <0.001 | 0.349 (0.259–0.471) | <0.001 |
| No smokers | 824 | 46.6 | 432 | 35.4 | 392 | 71.4 | Ref. | Ref. | ||
| Alcoholism | ||||||||||
| No | 1259 | 71.2 | 764 | 62.6 | 495 | 90.2 | Ref. | Ref. | ||
| Yes | 476 | 26.9 | 426 | 34.9 | 50 | 9.1 | 0.181 (0.132–0.248) | <0.001 | 0.304 (0.208–0.445) | <0.001 |
| Unknown | 34 | 1.9 | 30 | 2.5 | 4 | 0.7 | 0.206 (0.072–0.588) | 0.003 | 0.287 | |
| Drug use | ||||||||||
| No | 1609 | 91.0 | 1080 | 88.5 | 529 | 96.4 | Ref. | Ref. | ||
| Yes | 160 | 9.0 | 140 | 11.5 | 20 | 3.6 | 0.292 (0.180–0.471) | <0.001 | 0.939 | |
| HIV infection | ||||||||||
| No | 1585 | 89.6 | 1090 | 89.3 | 495 | 90.2 | Ref. | Ref. | ||
| Yes | 52 | 2.9 | 43 | 3.5 | 9 | 1.6 | 0.461 (0.223–0.953) | 0.037 | 0.822 | |
| Unknown | 132 | 7.5 | 87 | 7.1 | 45 | 8.2 | 0.497 | 0.355 | ||
| Immunosuppression | ||||||||||
| No | 1502 | 84.9 | 1033 | 84.7 | 469 | 85.4 | Ref. | |||
| Yes | 184 | 10.4 | 129 | 10.6 | 55 | 10.0 | 0.712 | |||
| Unknown | 83 | 4.7 | 58 | 4.8 | 25 | 4.6 | 0.833 | |||
| Previous treatment | ||||||||||
| No | 1652 | 93.4 | 1133 | 92.9 | 519 | 94.5 | Ref. | Ref. | ||
| Yes | 117 | 6.6 | 87 | 7.1 | 30 | 5.5 | 0.193 | 0.762 | ||
| Localization of tuberculosis | ||||||||||
| Pulmonary | 1382 | 78.1 | 1003 | 82.2 | 379 | 69.0 | 0.482 (0.382–0.609) | <0.001 | 0.296 | |
| Pleural | 241 | 13.6 | 166 | 13.6 | 75 | 13.7 | 0.975 | |||
| Disseminated | 125 | 7.1 | 83 | 6.8 | 42 | 7.7 | 0.520 | |||
| Extrapulmonary only | 185 | 10.5 | 90 | 7.4 | 95 | 17.3 | 2.627 (1.930–3.576) | <0.001 | 2.075 (1.395–3.084) | <0.001 |
| Diagnostic delay (days) | ||||||||||
| Median; IQR | 62 | 30–120 | 61 | 30–115 | 64 | 31–134 | 0.075 | 0.623 | ||
| Medical judgement | ||||||||||
| Compliant patient | 1558 | 88.1 | 1059 | 86.8 | 499 | 90.9 | Ref. | Ref. | ||
| Non-compliant patient | 78 | 4.4 | 67 | 5.5 | 11 | 2.0 | 0.348 (0.183–0.665) | 0.001 | 0.123 | |
| Unknown | 133 | 7.5 | 94 | 7.7 | 39 | 7.1 | 0.521 | 0.562 | ||
| Treatment outcome | ||||||||||
| Cured | 634 | 35.8 | 467 | 38.3 | 167 | 30.4 | Ref. | Ref. | ||
| Completed treatment | 565 | 31.9 | 344 | 28.2 | 221 | 40.3 | 1.797 (1.407–2.294) | <0.001 | 0.523 | |
| Prolonged treatment | 364 | 20.6 | 252 | 20.7 | 112 | 20.4 | 0.134 | 0.136 | ||
| Default | 1 | 0.1 | 0 | 0 | 1 | 0.2 | – | – | ||
| Lost to follow-up | 32 | 1.8 | 28 | 2.3 | 4 | 0.7 | 0.091 | 0.191 | ||
| Covid periods | ||||||||||
| Pre-Covid | 1264 | 71.5 | 867 | 71.1 | 397 | 72.3 | Ref. | |||
| Post-Covid | 505 | 28.5 | 353 | 28.9 | 152 | 27.7 | 0.591 | |||
Values in bold: p-value < 0,05
IQR: interquartile range.
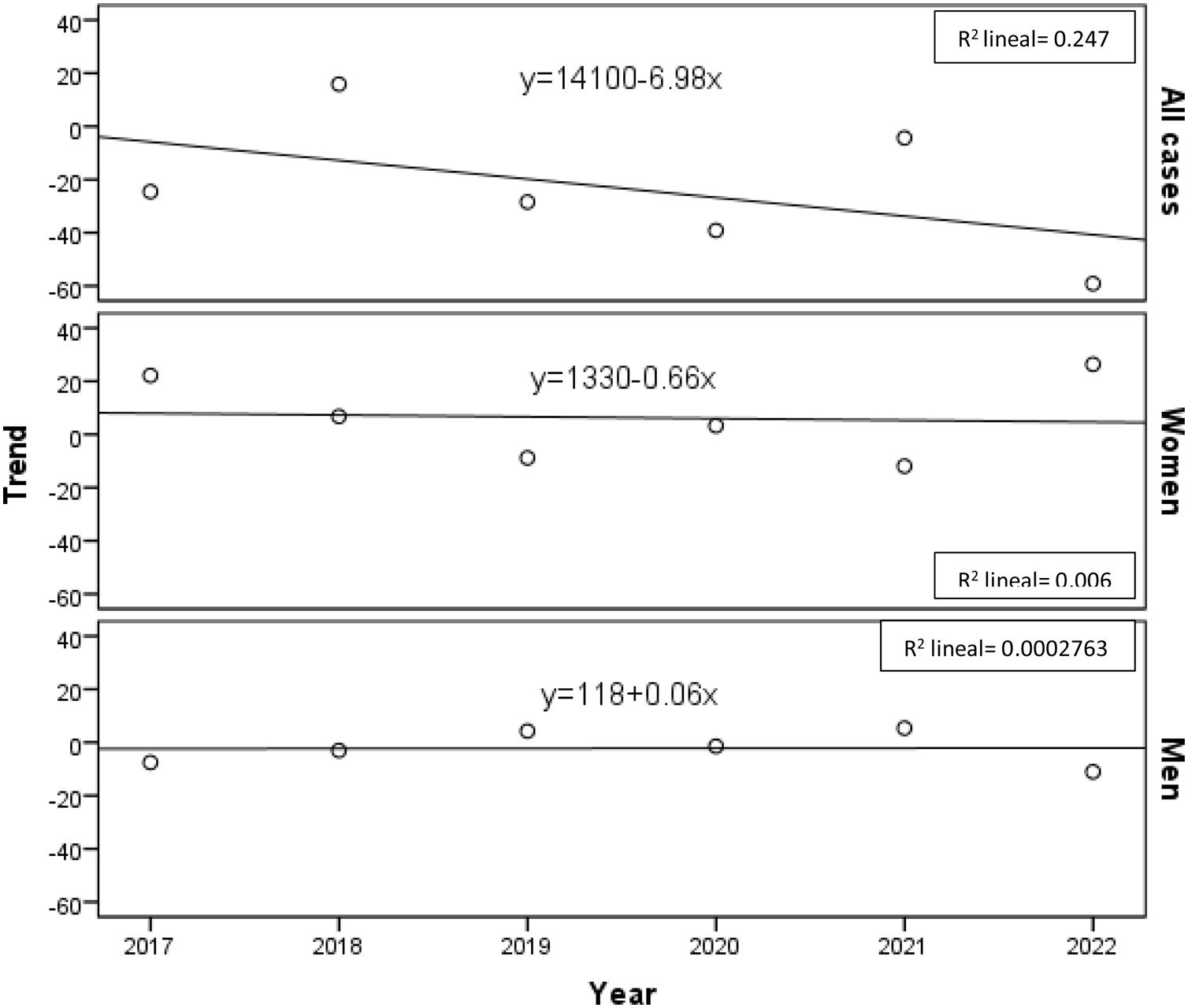
The annual incidence of cases has decreased significantly (y=14100−6.98x), although the linear trend shows that it is decreasing in women (y=1330−0.66x) while being positive in men (y=118+0.06x) (Fig. 1).
There have not been many studies on the relationship between gender and tuberculosis in Spain; nonetheless, certain data from national and autonomous TB control projects are accessible4–6 showing numbers between 39.6% and 40% of women and between 60% and 60.4% of men between 2015 and 2017. However, they do not study the factors to which they may be related.
The SEPAR PII-TB&MNT evaluation, conducted between 2006 and 2016, showed that the population studied had a significant declining trend in the number of cases in women. The percentage of cases among women in the last two years of the evaluation (2015–2016),7 was also lower than the figure reported in the World Health Organization's Global Tuberculosis Report 2019 (30.8% and 25.4% vs 32%),8 and the figures in our current study are also lower than those in the World Health Organization's Global Tuberculosis Report 2023 (31% vs 33%).9
A constraint of this research is that, apart from the variables examined here, we also need to consider other studies that have identified additional characteristics related to gender. One of them at University College London10 compared a short 4-month treatment to the 6-month standard and found gender differences in treatment outcomes without any objective biological causes. Others conclude that there is an urgent need for a greater understanding of gender-related barriers.11 Another study found evidence that, in low- and middle-income countries, men are more at risk and have less access to screening and diagnostic services.12 Some speculate that the development of tuberculosis may include a variety of physiopathological processes13 and according to some authors, biological factors, such as sex hormones and genetic factors, could contribute to the host's immunity during tuberculosis.14
Despite the decline in the inclusion of cases during the Covid pandemic15 (overload of medical services, possible reduction of cases due to the wearing of facemasks, decreased contact in public places or delayed diagnosis) and weakened TB control systems,16,17 it can be concluded that there are significant gender differences in the incidence, age, living situation, tobacco and alcohol consumption and the localization of tuberculosis patients and that the trend in the number of cases in women continues to decrease.
Ethical ApprovalThe Biomedical Research Ethics Committees of the different participating centres approved this study.
Authors’ ContributionsTeresa Rodrigo: conception and design of the study; acquisition, analysis and interpretation of data, and writing of the article.
Eva M. Tabernero, Luis Anibarro, José A. Gullón, Juan F Medina, Joan P. Millet, Marta M. García-Clemente, Joan A Caylà, José M. García-García: critical review of the intellectual content, final approval of the version presented.
Antonia Sáez: methodology design and statistical analysis of data. Working Group of the Integrated Tuberculosis and NMT Research Program (PII-TB & NMT): collection and contribution of data.
FundingGrant from the Spanish Society of Pulmonology and Thoracic Surgery (880/2019).
Conflicts of InterestThe authors declare no conflicts of interest.
Abigail Macías Paredes (Hospital Comarcal Sant Jaume de Calella); Adrián Sánchez Montalvá (Hospitales Vall d’Hebrón); Álvaro Cecilio Irazola (Hospital Universitario Lozano Blesa); Ángel Domínguez Castellanos (Hospital Universitario Virgen Macarena); Antón Penas Truque (Hospital Universitario Lucus Augusti); Antoni Soriano Arandes (Hospitales Vall d’Hebrón); Belén Mª Navas Bueno(Hospital General Básico Santa Ana); Dunibel Morillo (Hospital Ernest Lluch; Martín Elvira Pérez Escolano (Hospital del SAS de Jerez); Estefanía Sánchez Martínez (Parc Sanitari Sant Joan de Deu de Sant Boi); Francisco Sanz Herrero (Hospital General Universitario de Valencia); Guillermo J Pérez (Hospital Universitario de Gran Canaria “Dr. Negrín”), Igor Iturbe Susilla (Hospital Universitario de Basurto); Isabel López Aranaga (Hospital Universitario de Basurto); Isabel Santamaría Mas (Hospital de Txagorritxu); Isabel Suárez Toste (Hospital Universitario de Canarias); Israel Molina Pinagorte (Serveis Clinics de Barcelona); Javier Garros Garay (Hospital Santa Marina); Jonathan Cámara Fernández (Parc Sanitari Sant Joan de Deu); José Antonio Caminero Luna (Hospital Universitario de Gran Canaria “Dr. Negrín”); José David Cardoso Landivar (Hospital Universitario Vall d’Hebrón); José Luis Vidal Pérez (Complejo Hospitalario La Paz-Cantoblanco-Carlos III); Josefina Sabria Mestras (Hospital de Sant Joan Despí Moisès Broggi); Juan Diego Álvarez Mavárez (Hospital Carmen y Severo Ochoa); Juan Rodríguez López (Hospital San Agustín); Lander Altube Urrengoetxea (Hospital de Galdakao); Lydia Luque Chacón (Hospital de Sant Joan Despí Moisès Broggi); Mª Ángeles Jiménez Fuentes (Unitat de Tuberculosi Vall d’Hebrón-Drassanes); Mª Jesús Ruiz Serrano (Hospital General Universitario Gregorio Marañón); Mª Luisa de Souza Galvao (Unitat de Tuberculosi Vall d’Hebrón-Drassanes); Magnolia Nieto Marcos (Hospital Dr Moliner); María Somoza González (Consorcio Sanitario de Tarrasa); Marina Lumbierres Burgués (Serveis Clinics de Lérida); Miguel Santín Cerezales (Hospital Universitario de Bellvitge); Miguel Zabaleta Murgiondo (Hospital Universitario de Valdecilla); Neus Altet Gómez (Serveis Clinics de Barcelona); Pablo Fernández Álvarez (Hospital Álvarez-Buylla); Paloma Gijón Vidaurreta (Hospital General Universitario Gregorio Marañón); Rocío Martínez Gutiérrez (Hospital San Agustín de Avilés); Sarai Quirós Fernández (Hospital de Basurto); Silvia Dorronsoro Quintana (Hospital de Zumárraga); Vanesa Deya Vadel l (Hospital Son Llatzer); Virginia Pomar Solchaga (Hospital Universitario de la Santa Creu y Sant Pau); Xavier Casas García (Serveis Clinics de Barcelona); Yoel González Díaz (Serveis Clinics de Barcelona).
A complete list of the Integrated Tuberculosis Research Programme Working Group members is provided in Appendix A.