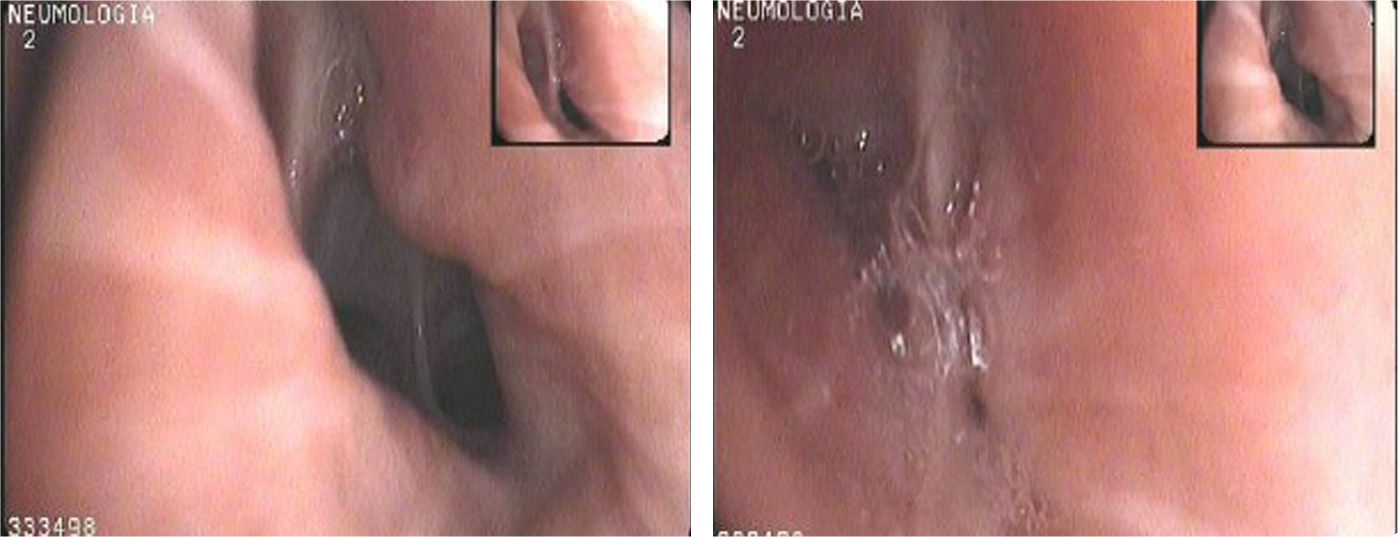
We present the case of an asthmatic patient with incapacitating symptoms that did not improve with optimized asthma treatment but responded well to continuous positive airway pressure (CPAP). The patient is a 71-year-old woman, never-smoker, hypertensive with a 40-year history of anxiety-depression syndrome. At the age of 65 she began to develop episodes of dry cough, dyspnea and wheezing. Spirometry was normal, skin prick tests for airborne allergens were negative and bronchial challenge testing with methacholine showed PC20 of 21mg/ml. The episodes of cough and dyspnea with wheezing became increasingly frequent and more severe. Spirometry was repeated, revealing mild obstruction and a post-bronchodilator test was positive. Treatment was initiated with high-dose inhaled corticosteroids, bronchodilators and anti-leukotrienes. Despite this, the patient frequently visited the emergency department and required long cycles of oral corticosteroids. She came to our specialized asthma clinic, where a head and neck CT was performed, that was normal. ENT examination ruled out vocal cord dysfunction. On bronchoscopy, the trachea and carina were normal but there was excessive dynamic airway collapse: collapsibility of >50% on expiration in the segmental and subsegmental bronchi of the RLL, RUL, LLL and to a lesser extent in the LUL (Fig. 1). Treatment with nasal CPAP at a pressure of 6cm H2O was prescribed during sleep and intermittently during the day. The patient progressed well, with good adaptation to CPAP and improved symptoms. She has not had to return to the emergency room, has discontinued her systemic corticosteroids, and remains controlled with moderate doses of inhaled corticosteroids.
Bronchomalacia is a defect of the composition of the cartilage of the bronchi, involving a loss of mechanical resistance. This means that the positive pressure developed during expiration narrows the lumen of the bronchi to a variable extent, making the passage of air difficult. This disorder is rare in adults and is usually caused by damage to the bronchial tree from chronic bronchitis, tuberculosis, prolonged intubation, surgery, injury, lung transplant or cancer.1 Chronic symptoms such as cough, dyspnea and recurrent infections occur. It is diagnosed by assessment of airway dynamics with tomography and fiberoptic bronchoscopy, and classified as mild, moderate or severe, depending on the degree of expiratory collapse.2 It can be localized or diffuse, affecting the trachea (tracheomalacia), the bronchi (bronchomalacia) or both (tracheobronchomalacia).3,4
The primary aim of treatment is to manage concomitant disease, and if there is no improvement, the use of CPAP as a pneumatic stent can be considered. There are, however, few reports of adults treated in this way, and controlled studies are required to confirm the benefits of this approach. Intermittent CPAP with a nasal mask during the day and continuous application at night is recommended. There are no specific criteria for selecting the appropriate CPAP pressure in these patients. In some cases, positive pressure stabilizes the patient and serves as a bridging treatment to other alternatives, such as stenting of the airway or surgery.2 We believe that long-term CPAP will be suitable for our patient, since, for the moment at least, this is providing satisfactory results.
Please cite this article as: Sala A, Martínez Deltoro A, Martínez Moragón E. Asmática con broncomalacia y buena respuesta al tratamiento con presión positiva continua en la vía aérea. Arch Bronconeumol. 2014;50:207–208.