Uveal melanoma (UM), constituting only 5% of primary melanomas,1 is a rare intraocular malignancy with aggressive potential, primarily affecting individuals aged 50–70.2 While metastasis at initial diagnosis is infrequent,1,3,4 almost 50% of patients develop metastatic disease, with the liver being the predominant site. We present a case of UM manifesting as a pulmonary mass with mediastinal nodes and bone metastases, mimicking lung cancer, diagnosed through Endobronchial Ultrasound (EBUS).
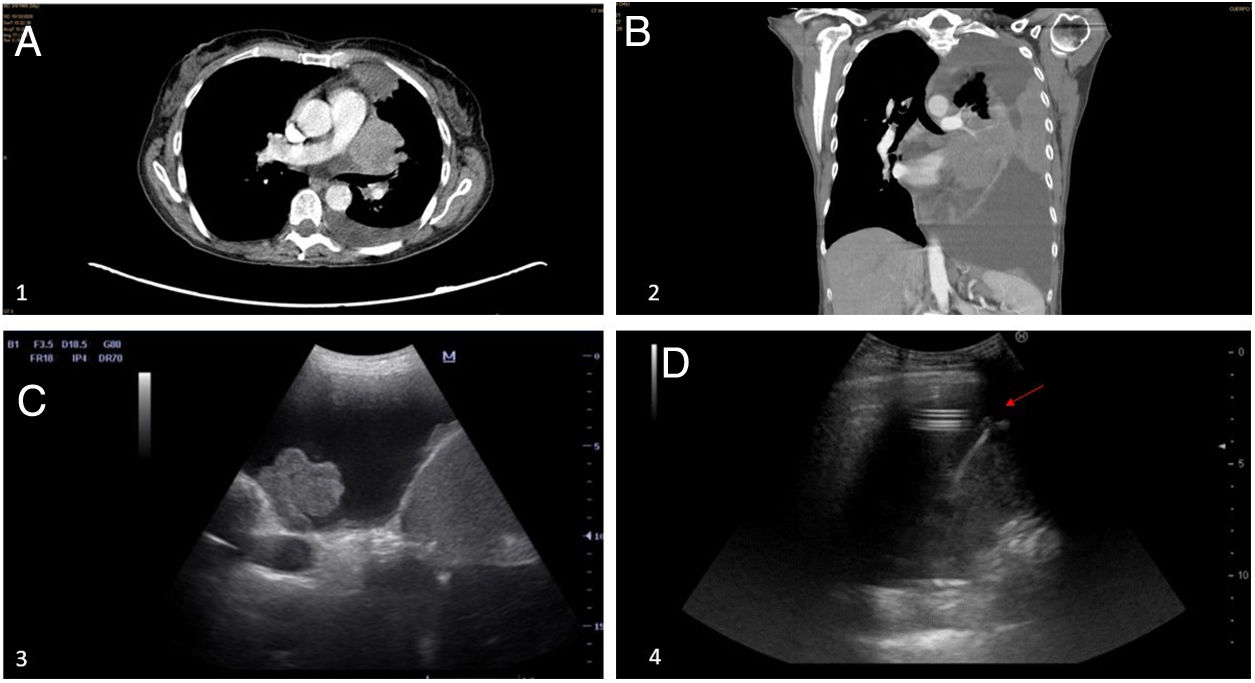
A 54-year-old woman with a light smoking habit and no significant medical issues seeking emergency care due to persistent dyspnea and fever. Imaging by Computed Tomography (CT) and Positron Emission Tomography-CT (PET-CT) scan revealed a 45mm×61mm central mass in the left upper lobe invading the mediastinum and multiple bilateral mediastinal adenopathies with high metabolic activity. EBUS-guided Fine Needle Aspiration (FNA) of the pulmonary mass confirmed Melanoma, revealing NRAS exon 3 mutation. Further examinations ruled out alternative primary sites, yet an ophthalmological evaluation identified a ciliary body lesion consistent with iris-ciliary body melanoma. Immunotherapy with Ipilimumab+Nivolumab was initiated. However, disease progression prompted the placement of an Indwelling Pleural Catheter (IPC), and severe pharmacological toxicity ensued. Regrettably, the patient succumbed to the condition five months post-diagnosis (Fig. 1).
We present a rare presentation of UM with initial pulmonary and lymph node metastases, a deviation from the usual hepatic involvement seen in metastatic UM. EBUS-TBNA, not previously described for UM, played a pivotal role in confirming the diagnosis and identifying mutations, showcasing its utility beyond traditional applications. At the time of diagnosis, our patient demonstrated atypical metastases in the lungs and lymph nodes, resembling lung cancer, contrasting the typical hepatic involvement in most cases.1 The patient's lack of hepatic metastasis despite extra-hepatic involvement was notable.
EBUS-TBNA, a well-established tool for assessing mediastinal and hilar lymph nodes, proved effective in detecting metastatic melanoma and identifying mutations.5 In our case, NRAS mutation, MelanA, and HMB45 were detected, guiding the choice of immunotherapy over other interventions due to the known poor response associated with NRAS mutations.4
Metastatic UM carries a grim prognosis, with a median survival of 6 months to 2 years.1,4 Our patient's disseminated disease precluded surgical intervention, emphasizing the prioritization of systemic treatment to extend survival. While primary tumor therapy does not significantly impact survival, it may alleviate symptoms.3 In our case, the patient's pulmonary symptoms were managed with an IPC, reflecting the importance of tailoring interventions to the individual's clinical presentation.
This case highlights the necessity of considering rare metastatic patterns in UM presentations. The use of EBUS-TBNA for diagnosing UM, especially with atypical metastases, expands its diagnostic potential. To our knowledge, this is the first reported case of UM presenting as a pulmonary mass and lymph node metastases diagnosed by EBUS. Comprehensive diagnostic approaches are crucial for accurate and timely management in such exceptional cases.
FundingNone declared.
Conflict of InterestsNo conflict of interests.