Trauma is the leading cause of mortality in children over one year of age in industrialized countries. In this retrospective study we reviewed all chest trauma in pediatric patients admitted to Mansoura University Emergency Hospital from January 1997 to January 2007. Our hospital received 472 patients under the age of 18. Male patients were 374 with a mean age of 9.2±4.9 years. Causes were penetrating trauma (2.1%) and blunt trauma (97.9%). The trauma was pedestrian injuries (38.3%), motor vehicle (28.1%), motorcycle crash (19.9%), falling from height (6.7%), animal trauma (2.9%), and sports injury (1.2%). Types of injuries were pulmonary contusions (27.1%), lacerations (6.9%), rib fractures (23.9%), flail chest (2.5%), hemothorax (18%), hemopneumothorax (11.8%), pneumothorax (23.7%), surgical emphysema (6.1%), tracheobronchial injury (5.3%), and diaphragm injury (2.1%). Associated lesions were head injuries (38.9%), bone fractures (33.5%), and abdominal injuries (16.7%). Management was conservative (29.9%), tube thoracostomy (58.1%), or thoracotomy (12.1%). Mortality rate was 7.2% and multiple trauma was the main cause of death (82.3%) (P<.001). We concluded that blunt trauma is the most common cause of pediatric chest trauma and often due to pedestrian injuries. Rib fractures and pulmonary contusions are the most frequent injuries. Delay in diagnosis and multiple trauma are associated with high incidence of mortality.
Los traumatismos son la primera causa de mortalidad en los niños de más de un año de edad en los países industrializados. En este estudio retrospectivo hemos revisado todos los traumatismos torácicos en pacientes pediátricos ingresados en el centro de urgencias del Mansoura University Emergency Hospital entre enero de 1997 y enero de 2007. Nuestro hospital recibió a 472 pacientes de menos de 18 años de edad. Hubo 374 pacientes varones, con una media de edad de 9,2±4,9 años. Las causas fueron traumatismos penetrantes (2,1%) y traumatismos cerrados (97,9%). Consistieron en traumatismos sufridos por peatones (38,3%), accidentes de vehículos a motor (28,1%), choques de motocicletas (19,9%), caídas desde una altura (6,7%), traumatismos causados por animales (2,9%) y lesiones deportivas (1,2%). Los tipos de lesión fueron contusiones (27,1%) y laceraciones pulmonares (6,9%), fracturas costales (23,9%) y volet costal (2,5%), hemotórax (18%), hemoneumotórax (11,8%), neumotórax (23,7%), enfisema quirúrgico (6,1%), lesiones traumáticas traqueobronquiales (5,3%) y lesión traumática del diafragma (2,1%). Las lesiones asociadas consistieron en traumatismos craneales (38,9%), fracturas óseas (33,5%) y traumatismos abdominales (16,7%). El tratamiento consistió en un enfoque conservador (29,9%), un tubo de toracostomía (58,1%) o una toracotomía (12,1%). La tasa de mortalidad fue del 7,2%, y los politraumatismos fueron la principal causa de muerte (82,3%) (p<0,001). Nuestra conclusión es que los traumatismos cerrados son la causa más frecuente de traumatismo torácico en los niños y que a menudo se producen en atropellos de peatones. Las fracturas costales y las contusiones pulmonares son los tipos de traumatismos más frecuentes. El retraso en el diagnóstico y los politraumatismos se asocian a una incidencia elevada de mortalidad.
Trauma is the first cause of mortality in children over the age of 1 in industrialized countries.1 Mortality from thoracic trauma reaches 30%, and its incidence diminishes as children get older.2 This holds true despite the fact that thoracic trauma represents only 4%–12% of the total number of hospitalizations due to trauma and that, alone, its mortality is low (6%–10%).3 The incidence of thoracic injury identified during the secondary examination indicates that pneumothorax/hemothorax and lung contusion are rather frequent in pediatric trauma (from 30% to 50% of patients with chest trauma), while cardiac contusions and traumatic injuries to the tracheobronchial tree, aorta, esophagus and diaphragm are relatively infrequent.4,5
Our objective was to evaluate the experience in our center regarding closed or penetrating pediatric chest trauma, their diagnosis, different treatment techniques and the clinical results obtained in these cases in our emergency hospital department, which is a tertiary reference center.
Patients and MethodsA retrospective study was completed for all chest traumas in pediatric patients who came to the emergency center at Mansoura University Emergency Hospital between January 1997 and January 2007. We obtained data on patient demographics, lesions, treatment, diagnostic explorations and the clinical results from the patient medical files. We excluded patients who had previously been hospitalized elsewhere in whom the initial surgical treatment had been done in other centers.
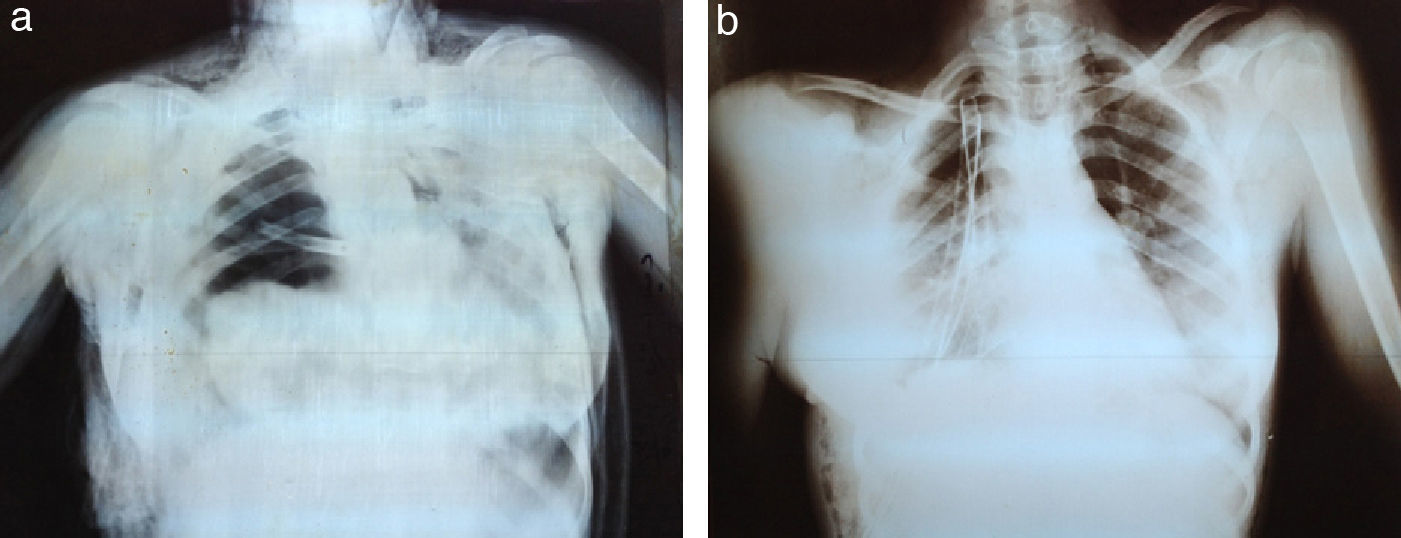
After the initial physical examination and the vital signs had been stabilized, chest x-rays were taken in all patients. Thoracic trauma was diagnosed with the chest radiographs ordered upon admittance and during the course of the patients’ hospitalizations. In children with an abnormal mediastinal silhouette, chest computed tomography (CT) was ordered.
Associated lesions were identified with other explorations, such as abdominal ultrasound in children who were suspected of abdominal trauma or who had pain during the abdominal palpation of the physical examination. In children who presented evident cranial trauma or were unconscious, cranial CT was ordered. In these patients, thoracic CTs were also taken. Rigid bronchoscopy was systematically performed in all cases with suspicion for tracheobronchial trauma.
Treatment of trauma patients was based on their state. Conservative treatment was used in cases of simple rib fractures, some cases of pulmonary contusion, cases of minimal pulmonary laceration and some cases of surgical emphysema. Thoracostomy tubes were used in cases of hemothorax, pneumothorax higher than 20%, hemopneumothorax and cases of massive surgical emphysema requiring mechanical ventilation.
Thoracotomy was done in patients with massive hemothorax and hemodynamic instability and in cases where more than 3ml/kg of body weight was drained for 3 consecutive hours. Thoracotomy was also indicated in cases of evident tracheobronchial traumatic injury on diagnostic bronchoscopy, diaphragmatic rupture or traumatic thoracotomy.
The statistical analysis was done with the SPSS statistical program (SPSS 15 Inc., Chicago, IL, USA). The Shapiro–Wilk test was used to evaluate the normal character of the distribution. The continuous variables with normal distribution were presented as mean±standard deviation. The continuous data without normal distribution were presented as median and range. The discrete variable data were presented as number and/or frequency.
ResultsBetween January 1997 and January 2007, our hospital received a total of 472 pediatric patients with chest trauma. The proportion of male:female patients was 3.81:1 (374 boys and 98 girls). Mean patient age was 9.2±4.9.
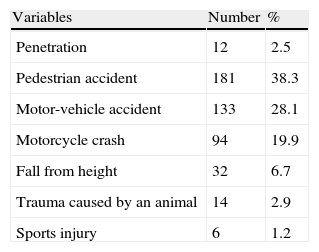
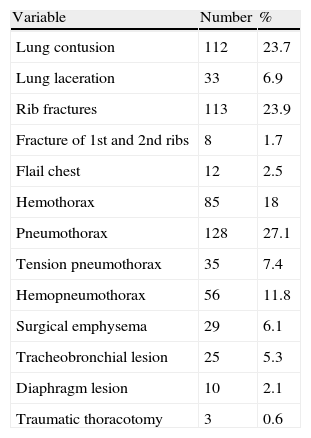
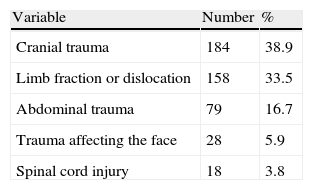
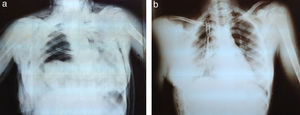
We observed penetrating trauma in 12 patients (2.1%): stab wounds (7 patients), falls on a sharp object (3 patients) and bullet wounds (2 patients). The most frequent causes of closed trauma were pedestrian accidents, seen in 181 patients (38.3%) (Table 1). Pulmonary trauma lesions consisted of contusions or lacerations, and the rib fractures went from simple cases to cases of flail chest. Tracheobronchial lesions were observed in 5.3% of the cases (Fig. 1), diaphragm lesions in 2.1%, and there were traumatic thoracotomies in 0.6% (3 cases) (Table 2). The associated traumatic lesions were very frequent, especially cranial trauma, which was present in 184 patients (38.9%). The incidence of multi-organ lesions was 64.4% (304 patients), while 202 children (42.3%) had affectation of 3 or more systems (Table 3).
Types of Chest Trauma.
| Variable | Number | % |
| Lung contusion | 112 | 23.7 |
| Lung laceration | 33 | 6.9 |
| Rib fractures | 113 | 23.9 |
| Fracture of 1st and 2nd ribs | 8 | 1.7 |
| Flail chest | 12 | 2.5 |
| Hemothorax | 85 | 18 |
| Pneumothorax | 128 | 27.1 |
| Tension pneumothorax | 35 | 7.4 |
| Hemopneumothorax | 56 | 11.8 |
| Surgical emphysema | 29 | 6.1 |
| Tracheobronchial lesion | 25 | 5.3 |
| Diaphragm lesion | 10 | 2.1 |
| Traumatic thoracotomy | 3 | 0.6 |
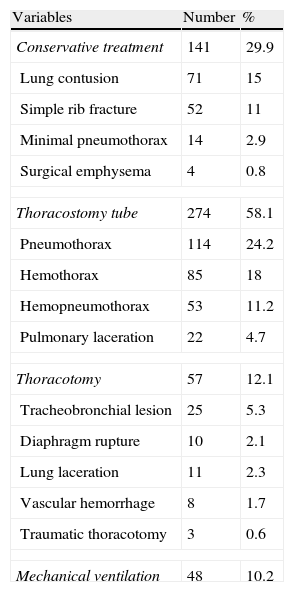
Conservative treatment (observation) was used in 141 patients (29.9%). Supplemental oxygen was necessary in 18 cases. The use of a thoracostomy tube was indicated in 274 cases of hemothorax (58.1%), apart from the patients who underwent thoracotomy, which was done in 57 patients (12.1%) (Table 4).
Treatment of Chest Trauma.
| Variables | Number | % |
| Conservative treatment | 141 | 29.9 |
| Lung contusion | 71 | 15 |
| Simple rib fracture | 52 | 11 |
| Minimal pneumothorax | 14 | 2.9 |
| Surgical emphysema | 4 | 0.8 |
| Thoracostomy tube | 274 | 58.1 |
| Pneumothorax | 114 | 24.2 |
| Hemothorax | 85 | 18 |
| Hemopneumothorax | 53 | 11.2 |
| Pulmonary laceration | 22 | 4.7 |
| Thoracotomy | 57 | 12.1 |
| Tracheobronchial lesion | 25 | 5.3 |
| Diaphragm rupture | 10 | 2.1 |
| Lung laceration | 11 | 2.3 |
| Vascular hemorrhage | 8 | 1.7 |
| Traumatic thoracotomy | 3 | 0.6 |
| Mechanical ventilation | 48 | 10.2 |
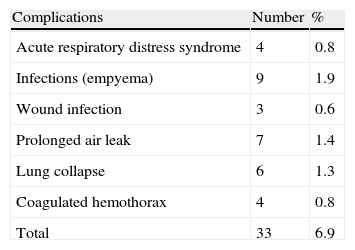
Complications were observed in 33 patients (6.9%) (Table 5). The mortality rate was 7.2% (34 patients), and it was related with the severity of the associated lesions. Death occurred due to thoracic causes alone in 6 patients (17.6%). One of the cases was due to a penetrating cardiac wound in a patient who arrived with no pulse. The patient was examined, revived and treated with mechanical ventilation for 5 days, with no signs of recovery. Three fatally injured patients had suffered extensive pulmonary lacerations. The two remaining fatal cases were due to tracheobronchial lesions. Polytrauma was the cause of death in 28 patients (82.3%) (P<.01). The polytrauma deaths were due to associated cranial trauma in 20 patients (58.8%) and abdominal trauma in 8 patients (23.5%).
DiscussionMansoura University Emergency Hospital is a tertiary reference center for trauma patients in Egypt that treats the population in the Dakahlia district and adjacent areas. This center specialized in trauma patients serves approximately 15 million people. Trauma is the first cause of death in the pediatric population, and most trauma lesions in childhood are due to closed contusions. The frequency of thoracic injury in children can reach 50% in cases of polytrauma.6–8
Generally, boys are more likely to have trauma injuries than girls due to their greater tendency towards participating in outdoor activities. In our study, the boy:girl ratio was 3.81:1. This result concurs with the 4:1 ratio reported by Bickford in a series of 26 children and adolescents from Liverpool with chest trauma7 and the 3.3:1 ratio from Kilman and Charnock.9 Balci et al. and Smyth, however, have reported a proportion of approximately 2 boys for every girl.4,10
Most pediatric chest trauma (80%–90%) is closed trauma. In our study, closed trauma represented 98% of the total. Motor vehicle accidents were the main cause of these contusion traumas. Most children receive this type of trauma as pedestrians who are hit by cars (26%–72% of cases). In our study, 38.8% of the patients included had pedestrian trauma. This incidence is similar to that reported by Peterson et al., which indicated 35% pedestrian trauma,11 while this number reached 68% in the study by Smyth.10 In our study, motor vehicle accidents were 28.1%, which concurs with what has been observed in other studies that have reported an incidence of 2%–34%. This contrasts with what is observed in adults, in whom most accidents affect vehicle occupants.2,5,6,8,12,13
Other mechanisms are bicycle accidents, which in many series have been observed to affect 4%–14% of cases,9–13 compared with our percentage of 19.9%. High falls are between 5% and 18% in many studies,5–8,10 and in our case the incidence was 6.7%. Penetrating trauma greatly depends on age and area. In our study, 2.1% of the cases were penetrating trauma, which is similar to Nakayama's report of 2.9%,5 but meanwhile this percentage was 12% in the study by Peclet et al.3
A fast diagnosis of thoracic injury is often difficult because the symptoms may not appear until after a few hours.2–5 Moreover, simple chest radiography in supine decubitus may not detect or may underestimate 38% of the lesions that are visible in the thoracic planes of abdominal CT. There may be atelectasis, parenchymal lacerations, traumatic lung cysts and pneumothorax, although these may not be evident in the initial radiographic examination.3 During CT to evaluate possible abdominal lesions, the inclusion of several thoracic planes may improve the diagnosis of the existing lesions and contribute to modifying treatment methods in order to improve clinical results.4
Children differ from adults because of their greater ribcage flexibility. This explains the lower incidence of flail chest and rib fractures in the population of that age group. In 90% of cases in which there was a demonstrated existence of vital intrathoracic injuries, there were no fractures.11 In our study, there were rib fractures in 23.9% of cases, which is a percentage similar to that reported by Garcia et al. in 199014 and by Meller et al. in 1984.15 On the other hand, the Nakayama group and Inan et al. observed an incidence of 51% and 62%, respectively, of rib fractures in their patients.5,12
Pulmonary contusion is the most frequent chest trauma injury in children, with an incidence of 40%–73%. It was seen in 128 (27.1%) of the children in our study, which is a percentage similar to the report by Balci, who observed lung contusions in 37 out of 137 (27%) children.4 On the other hand, Nakayama et al. and Smyth observed an incidence of pulmonary contusions of 53.3% and 56%, respectively.5,10 In our study, the incidence of pneumothorax was 23.7%. In other reviews, this incidence has oscillated between 12% (Peclet et al.) and 38% (according to what is described Nakayama et al.). Our incidence of hemothorax (18%) coincides with that of Balci (18.2%), while the incidence observed in other studies has gone from 4% in the study by Smyth or 14% in those by Nakayama et al. and Peclet et al., to 39% according to the data by Black et al. and Inan et al.3–6,10,12
The presence of a tracheobronchial lesion should be suspected in cases of persistent subcutaneous emphysema and pneumothorax, despite the presence of properly functioning thoracic tubes. An emergency bronchoscopy should be done to confirm this diagnosis, which is very uncommon in children. The incidence of tracheobronchial lesions in our study is 5.3%, which is similar to the incidence reported by Smyth (5%), while Nakayama and Balci indicated lower incidences (2.9% and 1.4%, respectively).4,5,10 The rupture of the diaphragm is more frequent on the left side. We should suspect its presence when a child has been crushed. This incidence of diaphragm rupture in our study is 2.1%, similar to the reports by Balci et al. (2.9%) and Smyth (3%).4,10
Associated extrathoracic trauma lesions are frequent but they are not affected by age. These injuries make a significant contribution towards mortality. Cranial trauma is the most frequently recorded extrathoracic trauma (64% in adults, 83% in children). In our study, this incidence is 38.9%, which corresponds with the study by Nakayama et al., who observed cranial trauma in 37% of their patients. Meanwhile, Smyth and Balci et al. observed lower incidences of cranial trauma (20% and 26%, respectively).4,5,10
Intra-abdominal lesions are seen in approximately 50% of adults and children, with a notable increase in splenic injuries in this latter group. We have observed an incidence of 16.7% of lesions of this type, while the incidence reported by other authors ranges between 10% described by Smyth or 11% by Balci et al. and 23% observed by Nakayama et al. In our study, osteoarticular trauma was seen in 33.5% of the cases, which agrees with reports from Nakayama et al., who observed them in 38% of patients, while Smyth and Balci et al. described an incidence of 21%.4,5,9
The use of thoracotomy is very infrequent and is only indicated in cases of persistent hemorrhage through the thoracic drain, a high suspicion of mediastinal lesion or uncontrollable shock. The overall percentage of thoracic trauma requiring surgery is around 5%–10%.14,15 In our study, thoracotomy was used in 12.1% of patients; in 8 cases (66%) there were penetrating causes. Although penetrating traumas are a low percentage of chest injuries, they are the cause of a high proportion of thoracotomies.3,5 Peterson et al. observed a lack of difference in the frequency of thoracotomies due to closed trauma in children, adolescents and adults (2%–8%). However, in the cases of penetrating wounds, the incidence of thoracotomy in children (40%) was more than double of what was seen in other age groups.11
The rate of mortality due to thoracic trauma ranges between 6.7% and 25%.4,5,16,17 In our case, the mortality rate (7.2%) was within these limits. Mortality in children with isolated chest trauma in our study was 17.6%, compared with 23.5% for chest and abdominal trauma and 58.8% for cranial and chest trauma. Peclet et al. described a mortality rate of 26% and the presence of multisystem trauma lesions in 82% of patients.3 Rielly et al. indicated that 25% of patients with closed trauma died, generally as a consequence of associated cranial trauma.16 Nakayama et al. indicated that 68% of their patients with chest trauma also presented extrathoracic trauma injuries, with a mortality rate of 7%.5
Our conclusion is that closed trauma is the most frequent chest trauma seen in children, and that this type of trauma is often caused by pedestrian accidents. Rib fractures and lung contusions are the most frequent types of trauma. Delayed diagnoses and polytrauma are associated with a high incidence of mortality.
Conflict of InterestsThe authors declare having no conflict of interests.
☆ Please cite this article as: Ismail MF, al-Refaie RI. Traumatismos torácicos en niños: experiencia de un centro. Arch Bronconeumol. 2012;48:362–6.