A 16-year-old male was referred to the paediatric pulmonology clinic for suspected cystic lung disease on imaging tests.
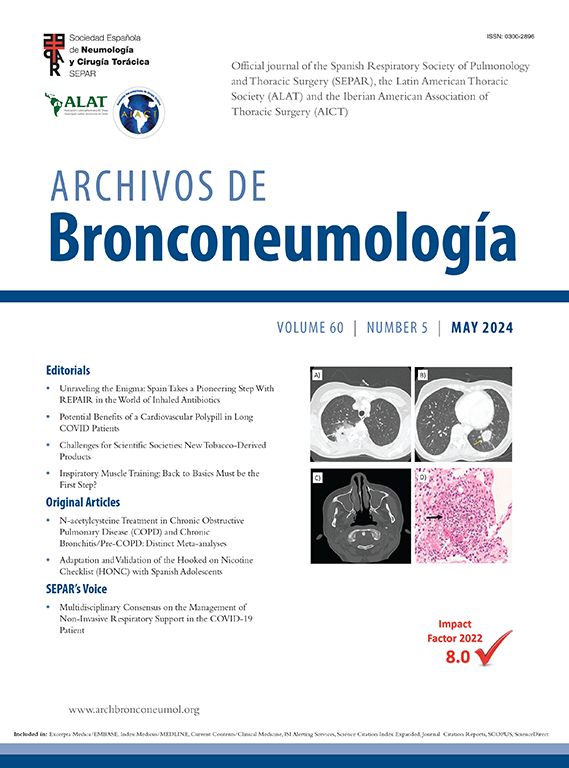
The patient arrived to the consultation suffering from tenosynovitis in the left carpus and asthenia since a couple of months. The initial assessment showed stage IV renal failure (GFR 29.48mL/min), and therefore a renal biopsy (Fig. 1) was performed. Results showed evidence of pauci-immune crescentic glomerulonephritis concordant with ANCA-associated vasculitis (AAVs) which is why it was decided to complete the study, among others, with a full-body computed tomography scan (CTs). At the pulmonary level, multiple subpleural and peri-fissural pulmonary cysts were observed together with small, low-density, centrolobulillary pulmonary nodules (Fig. 1). Respiratory function tests showed moderate restrictive ventilatory impairment (FVC 2.57L (64%), FEV1 2.50L (76%), FEV1/FVC 0.97) and moderate diffusion impairment (DLCO) 45%.
(A) Renal biopsy with crescents. (B–D) Thoracic computed tomography with multiple subpleural pulmonary cysts, small, peripheral and in cystic of small size, peripheral and in fissures arranged in a single row. Multiple small, low-density, centrolobulillary pulmonary nodules with mosaic pattern.
Laboratory tests showed elevated titres of anti-MPO antibodies (739IU/mL) and rheumatoid factors (247IU/mL), while all other autoimmunity markers tested negative (DNAdc, Rib-P, PCNA, U1-RNP, anti-Ro, anti-La, Scl-70, CENP-B, Fibrillarin, RNA Polymerase III, Jo-1, Mi-2, PM-Scl, anti-cardiolipin, lupus anticoagulant, antiB2 GPI, anti-proteinase 3, anti-transglutaminase, anti-glomerular basement membrane). Complement levels were normal, as were immunoglobulin classes and subclasses. Furthermore, looking at the patient's family health history, his mother had been diagnosed with probable lupus at the age of 18 and died of breast cancer at an early age.
Given the atypical pulmonary imaging in the context of vasculitis and considering the serological findings and the family history, the initial diagnosis was reconsidered, and the possibility of a genetic autoinflammatory/autoimmune syndrome with pulmonary involvement was contemplated. Among these, COPA syndrome was considered given it is characterised by the presence of pulmonary cysts, an autoantibody profile and renal involvement, which are all symptoms that the patient experienced. The genetic study requested in light of this suspicion confirmed the diagnosis of COPA syndrome with the heterozygous genetic variant of the variant c.698G>A, p.Arg233His in the COPA gene. Given the initial diagnosis of AAVs, the patient received treatment with boluses of methylprednisolone and three doses of cyclophosphamide. Subsequently, in the absence of improvement, four doses of rituximab and seven sessions of plasmapheresis. The patient remained on rituximab as maintenance treatment (4 doses every 6 months) until the diagnosis of COPA syndrome. This was followed by a plasma interferon signature, with 28 z-score positive 15.8 and 6 z-score positive 16.44. For this reason, ruxolitinib was added and the interferon signature was repeated after 6 months, verifying a significant decrease, with a 28 z-score positive 3.87 and 6 z-score positive 3.38. The patient remained stable without infectious complications, until he finally underwent renal transplantation. Regarding the respiratory, since diagnosis, there is no data of progression in imaging tests and there has been a slight improvement in respiratory function tests (FVC 3.14L (79%), FEV1 2.70L (82%), FEV1/FVC 0.86, DLCO 65%). A genetic study of relatives was performed, ruling out involvement in both the patient's father and brother. Due to the death of the mother there is no genetic information available about this parent, who could probably be the index case.
COPA syndrome is a newly recognised (since 2015) and rare monogenic autoimmune disorder. Clinical features include inflammation of the lungs, kidneys, and joints. It is inherited as an autosomal dominant, variably penetrant disease due to missense genetic variant in the COPA gene on chromosome 1.
The disease is characterised by pulmonary involvement in almost all cases, either as diffuse alveolar haemorrhage at an earlier age, or as interstitial lung disease at a later age. It can be diagnosed through a pattern of pulmonary cysts observed histologically in follicular bronchiolitis and on CTs. Patients with COPA syndrome also develop renal disease in 80% of the cases, and this is AAVs. Seventy-five percent of the patients show crescents in the renal biopsy. Arthritis is also a very common symptom and present in up to 95% of cases.
It is increasingly considered important to differentiate this syndrome from other frequent autoimmune diseases in order to perform a targeted treatment with JAK inhibitors, which are considered the maintenance treatment of choice, and to monitor it with the interferon signature. As for prognosis, there is insufficient data to date on the long-term evolution of these patients with treatment with JAK inhibitors, although there are documented cases of patients who have required renal transplantation, like our patient's case, or lung transplantation at variable ages.
The case presented is the first documented to date of this kind in Spain.1 It highlights the importance of achieving a correct diagnosis of diffuse parenchymal lung diseases in children due to the implications this may have in terms of finding out their adjust the treatment and offer the possibility of genetic counselling.
Conflict of InterestsThe authors state that they have no conflict of interests.