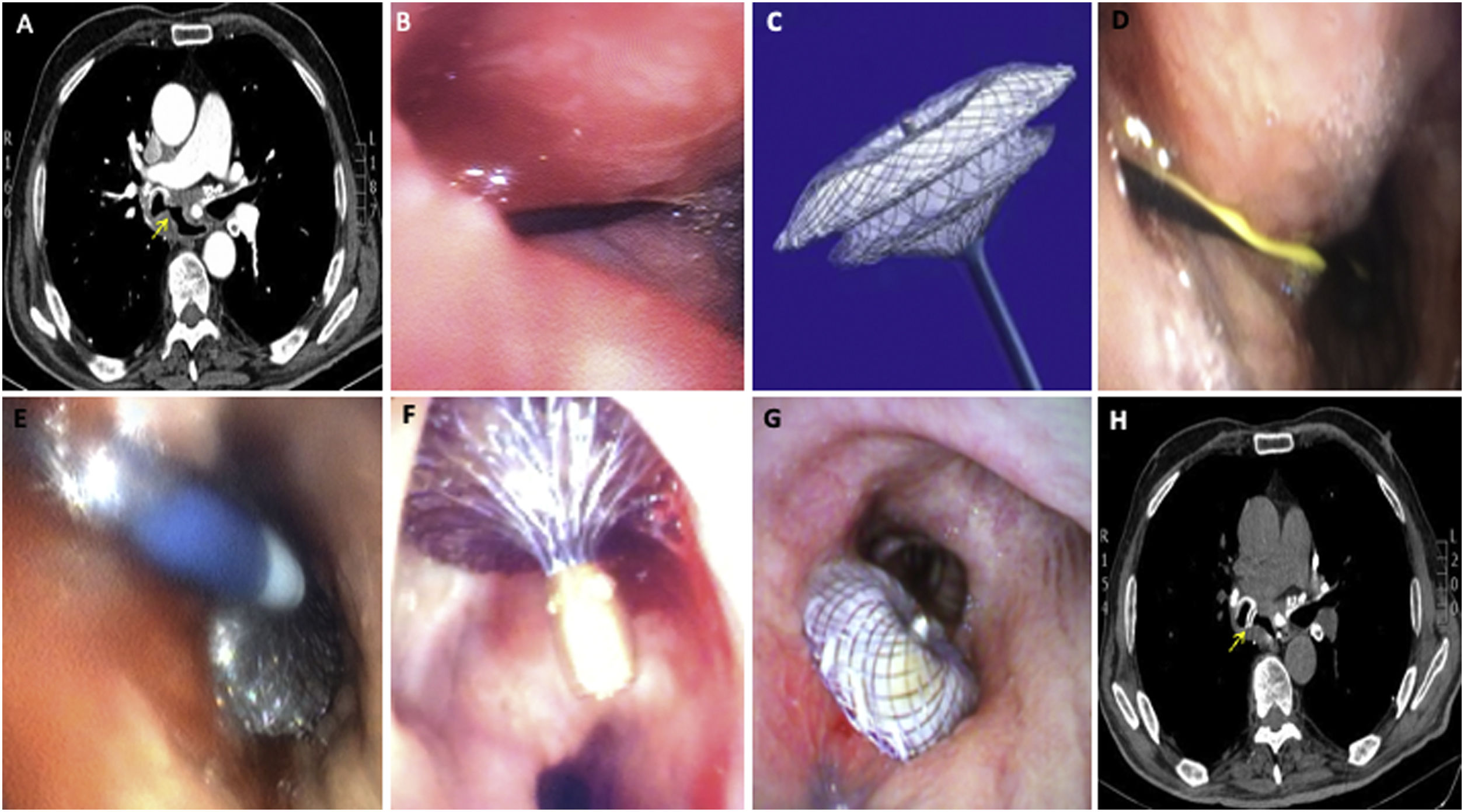
We report the case of a 70-year-old man admitted to our hospital for bilateral pneumonia and weight loss. Chest CT showed a large bronchoesophageal fistula associated with esophageal diverticulum (Fig. 1a). Bronchoscopy revealed a 2.5cm fistula in the medial wall of the intermediate bronchus (Fig. 1b). Surgical repair was ruled out because of the patient's current severe status. We decided to perform a hybrid procedure using bronchoscopy and simultaneous esophagoscopy with the aim of implanting an Amplatzer® to close the fistula (Fig. 1c); this device was designed primarily for percutaneous closure of congenital heart defects. During esophagoscopy, a guidewire was introduced through the fistula under bronchoscopy guidance (Fig. 1d). The device was released in the correct position (Fig. 1e). Complete sealing of the fistula was confirmed by esophagoscopy (Fig. 1f), bronchoscopy (Fig. 1g) and follow-up CT (Fig. 1h). The patient was discharged 3 weeks after placement of the device, and in the 4 months before withdrawal prior to definitive surgical repair he did not require hospitalization and did not develop any device-related complications. The recommended treatment of bronchoesophageal fistulas is esophageal stent placement, but we believe that whenever this is impossible or when the fistula is refractory to initial management, the Amplatzer should be considered, especially in patients with non-malignant chronic fistulas. This procedure may also be used in some cases as bridging therapy until definitive surgical repair, as occurred in our case.
(a) Large bronchoesophageal fistula visualized on computed tomography. (b) Bronchoscopy confirmed the 2.5cm fistula in the medial wall of the intermediate bronchus. (c) Amplatzer®. (d) Guidewire introduced through the fistula during esophagoscopy. (e) Successful release of the device. (f) Esophageal view of complete fistula closure. (g) Bronchoscopic view of complete fistula closure. (h) Complete fistula closure seen on follow-up computed tomography.