Although the number of lung transplants in Spain is increasing annually, more organs are required to ease waiting lists. Controlled non-heart beating donors (cNHBD) (Maastricht III) are a reality at international level, and contribute significantly to increasing donor numbers. In this study, we present our cNHBD protocol and the initial experience in Spain using lung grafts from this type of donor. Three bilateral lung transplants were performed between January 2012 and December 2014. Preservation was by ex vivo lung perfusion in 2 cases and by traditional cold perfusion in the other. None of the patients developed grade 3 primary graft dysfunction, no in-hospital mortality was recorded and 1-year survival was 100%. These initial results, and international experience, should help to develop similar protocols to encourage the use of controlled non-heart beating donors.
Aunque el número de trasplantes pulmonares en España es cada año mayor, es necesario aumentar el número de órganos disponibles para aliviar las listas de espera. Los donantes en asistolia controlada (DAC) (Maastricht III) son una realidad a nivel internacional y contribuyen significativamente a aumentar el número de donantes. En este trabajo presentamos nuestro protocolo de DAC y la experiencia inicial en España usando injertos pulmonares provenientes de este tipo de donantes. Desde enero 2012 a diciembre 2014, se han realizado 3 trasplantes pulmonares bilaterales. De ellos, en 2 casos se realizó preservación ex vivo y en el otro preservación tradicional en frío. Ninguno de los pacientes desarrolló disfunción primaria del injerto grado 3, no se registró mortalidad hospitalaria y la supervivencia al primer año fue del 100%. Estos resultados iniciales, y la experiencia internacional, deberían contribuir al desarrollo de protocolos similares para fomentar el aprovechamiento de los DAC.
Donor shortage is a problem that affects the waiting lists of all lung transplantation groups, so it is essential that all sources of potential donors are explored and that donors with expanded criteria (controlled and uncontrolled non-heart beating donors [NHBD], elderly donors and others), live donors and ex vivo perfusion techniques are considered.
Hardy et al.1 performed the first lung transplantation in 1963 using a non-heart beating organ. At the end of the 1990s, Egan et al.2 rekindled interest in non-heart beating lung donation, and Love et al.3 performed the first successful lung transplantation from an NHBD. Since then, this type of donation has become an additional, reliable source of organs in many countries, and has contributed to a significant rise in the number of transplantations with excellent outcomes.4–6
Nowadays, uncontrolled non-heart beating donors have become a reliaty, and has helped to increase the number of lung transplants performed.7,8 In view of this experience, backed up by the work of other groups, our hospital implemented a similar protocol with the aim of procuring NHBD grafts to increase our rate of lung transplantations.
Clinical ReportcNHBD protocol used in our hospital can be summarized as follows: after the patient's family has agreed to limitation of therapeutic efforts (LTE), organ donation is proposed. If family agrees, the patient is evaluated as a potential donor, and the same criteria as for brain death donors are applied.9
After all parameters have been examined, a bolus of 1000UI/kg heparin is administered and LTE starts generally in the operating room.
In our hospital, the maximum period between LTE and cardiac arrest (agonal phase) is set at 2h. If the heart does not stop beating during this period, the patient is returned to the intensive care unit. Warm ischemia time (WIT) is defined as the time between a fall in mean blood pressure to below 60mmHg and cold preservation through the pulmonary artery. A maximum of 60min WIT is accepted for the graft to be considered valid.
After asystolia, there is a observation period (5min) and the physician in charge of LTE certifies death. The patient is reintubated, and fibrobronchoscopy is used to ensure than no bronchial aspiration occurred during the agonal phase. At the same time, a median sternotomy is performed, and the pulmonary artery is catheterized for perfusion of a low-potassium dextran solution (Perfadex®). Grafts are inspected in the same manner as brain death donors.
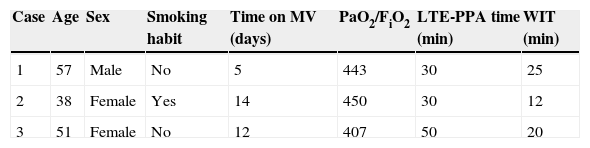
In terms of results, between January 2012 and December 2014, 26 patients were evaluated as possible donors after the family agreed to LTE. Of these, 23 were donors, of whom only 3 met criteria for lung donation. The outcomes of these lung transplant procedures are listed in Tables 1 and 2.
Donor Characteristics.
| Case | Age | Sex | Smoking habit | Time on MV (days) | PaO2/FiO2 | LTE-PPA time (min) | WIT (min) |
|---|---|---|---|---|---|---|---|
| 1 | 57 | Male | No | 5 | 443 | 30 | 25 |
| 2 | 38 | Female | Yes | 14 | 450 | 30 | 12 |
| 3 | 51 | Female | No | 12 | 407 | 50 | 20 |
LTE-PPA time: time between limitation of therapeutic efforts and cold flush perfusion through pulmonary artery, MV: mechanical ventilation, WIT: warm ischemia time.
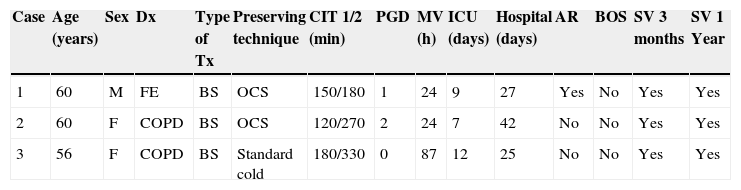
Characteristics of Recipients, Type of Transplant and Post-Operative Progress.
| Case | Age (years) | Sex | Dx | Type of Tx | Preserving technique | CIT 1/2 (min) | PGD | MV (h) | ICU (days) | Hospital (days) | AR | BOS | SV 3 months | SV 1 Year |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 60 | M | FE | BS | OCS | 150/180 | 1 | 24 | 9 | 27 | Yes | No | Yes | Yes |
| 2 | 60 | F | COPD | BS | OCS | 120/270 | 2 | 24 | 7 | 42 | No | No | Yes | Yes |
| 3 | 56 | F | COPD | BS | Standard cold | 180/330 | 0 | 87 | 12 | 25 | No | No | Yes | Yes |
AR, acute rejection; BOS, bronchiolitis obliterans; BS, bilateral sequential; CIT 1/2, cold ischemia time of first graft/second graft; COPD, chronic obstructive pulmonary disease; Dx, diagnosis; F, female; FE, Fibroemphysema; M, male; MV, mechanical ventilation; OCS, Organ Care System; PGD, primary graft dysfunction; SV, survival; Tx, transplant.
None of our graft recipients developed grade 3 or severe primary graft dysfunction (PGD), and there were no deaths during hospitalization or in the 30-day post-transplant period. Survival at 3 months and 1 year was 100%.
DiscussionControlled NHBD has led to a significant worldwide increase in donor numbers, providing PGD and survival outcomes comparable to those achieved with brain death donors.6 In our hospital, the results of the 3 lung transplants perfore with cNHBD were similar to those of other more experienced groups.
The first 2 donors were reevaluated using the ex vivo Organ Care System (OCS® Lung, TransMedics, Inc.). Grafts showed optimal functional and oxygenation parameters. Standard cold preservation was applied in the third case.
A controversial issue in the use of cNHBD is heparinization of the donor before LTE. We prefer to administer heparin before LTE to avoid any risk of pulmonary thromboembolism, including microclots.10 On the other hand, some groups obtain excellent outcomes with the administration of heparin after cardiac arrest.4
In conclusion, we present here the first 3 cases of cNHBD lung transplantation performed in Spain. Our excellent outcomes, added to the international experience, may be used in the implementation of cNHBD protocols in intensive care units throughout the country, with the aim of expanding the lung donor pool.
We thank all the members of the lung transplantation team (surgeons, pulmonologists, anesthetists, nursing and auxiliary staff) and the Transplant Coordination and Intensive Care Unit of the Hospital Universitario Puerta de Hierro-Majadahonda for their efforts and dedication.
Andrés Varela de Ugarte (Servicio de Cirugía Torácica)
Piedad Ussetti (Servicio de Neumología)
Mar Córdoba Peláez (Servicio de Cirugía Torácica)
David Gómez de Antonio (Servicio de Cirugía Torácica)
José Manuel Naranjo Gómez (Servicio de Cirugía Torácica)
José Luis Campo-Cañaveral de la Cruz (Servicio de Cirugía Torácica)
Silvana Crowley Carrasco (Servicio de Cirugía Torácica)
Lucas Hoyos Mejía (Servicio de Cirugía Torácica)
Daniel Valdivia Concha (Servicio de Cirugía Torácica)
Lidia Macías Sotuela (Servicio de Cirugía Torácica)
Francisco Javier Moradiellos Díez (Servicio de Cirugía Torácica)
Juan José Rubio Muñoz (Coordinación de Trasplantes)
Christian García Fadul (Servicio de Neumología)
Rosalía Laporta Hernández (Servicio de Neumología)
Miriam Aguilar Pérez (Servicio de Neumología)
Cristina García-Gallo (Servicio de Neumología)
Ana Isabel González Román (Servicio de Anestesiología y Reanimación)
Pelayo de Merlo Martínez (Servicio de Anestesiología y Reanimación)
María Reyes Iranzo Valero (Servicio de Anestesiología y Reanimación)
Members of the Lung Transplant Unit of the Hospital Universitario Puerta de Hierro-Majadahonda are available in the Appendix 1.
Please cite this article as: Campo-Cañaveral de la Cruz JL, Gómez de Antonio D, Hoyos-Mejía L, Pérez-Redondo M, Laporta-Hernández R, Varela de Ugarte A. Experiencia inicial en trasplantes pulmonares con donantes en asistolia controlada en España. Arch Bronconeumol. 2015;51:e45–e47.