A 55-year-old man presented with a history of vitiligo diagnosed and treated in childhood, pulmonary tuberculosis treated in adolescence and hospital admission 2 years ago for SARS-CoV-2 pneumonia and respiratory failure, requiring noninvasive mechanical ventilation. He consulted for a dry cough, pain in the right hemithorax, loss of appetite and unquantified weight loss of 1 year of evolution. Physical examination revealed extensive hypochromic spots secondary to vitiligo and pain on deep palpation in the right hypochondrium. Laboratory tests were strictly normal and a thoraco-abdomino-pelvic computed tomography showed a thickening of the tracheal wall, as well as a hepatic and a pancreatic lesion (Fig. 1A–D).
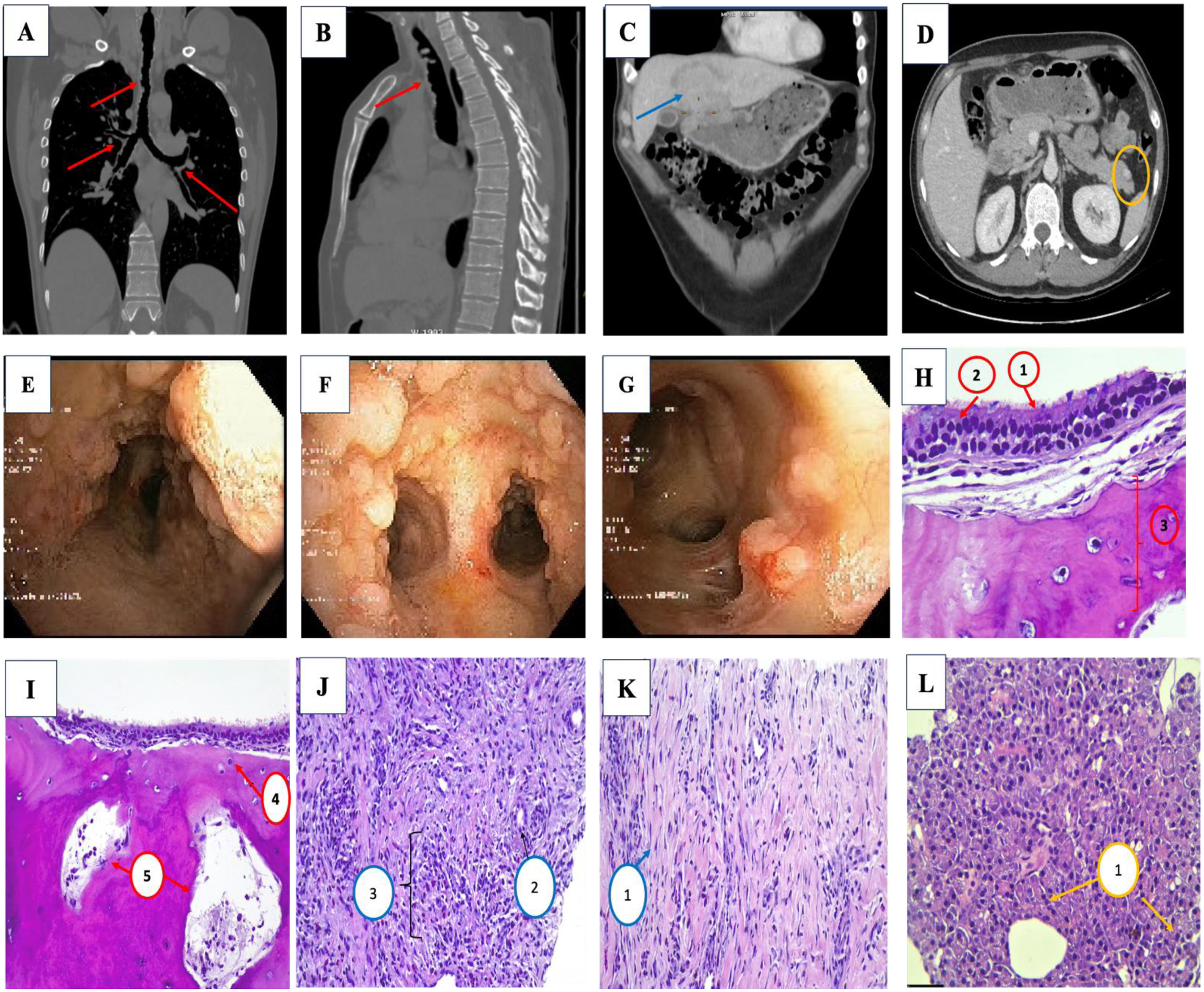
(A and B) Multiple foci of irregular mural thickening partially calcified in the trachea, in its two anterior thirds and with extension to the bronchial tree (red arrow). (C) Mass-like lesion in hepatic segment IV (blue arrow). (D) Lesion in the tail of the pancreas of approximately 11mm (yellow circle). (E–G) Polypoid lesions, petrosal, with scarce vascularization, without completely occluding the lumen of any bronchus, they respect the membranous the membranous side, more predominant in the trachea and main bronchi, which bronchi, decreasing in quantity until they are scarce at the level of segmental bronchi. (H) Respiratory type epithelium, formed by pseudostratified ciliated (1) and goblet cells (2) with presence of osteochondroblastic tissue in submucosa (3). (I) The bone component presents osteocytes (4), medullary cavities (5) and hematopoietic cellularity, surrounded by concentric lamellar bone matrix. (J and K) Proliferation of fibroblasts arranged in fascicles (1) encompassing some isolated bile duct (2). compatible with HIP. (L) Inflammatory infiltrate, with presence of lymphocytes, plasma cells, polymorphonuclear cells and eosinophils compatible with PNT (3).
A fibrobronchoscopy was performed, which revealed the presence of polypoid tracheobronchial lesions (Fig. 1E–G), biopsies were taken, the histopathological study being compatible with an osteochondroplastic tracheobronchopathy (OT) (Fig. 1H and I)
On the other hand, an echo-guided core needle biopsy of the hepatic lesion and an echo-endoscopy-guided fine needle puncture of the pancreatic lesion were performed. The cyto-histological study was consistent with a hepatic inflammatory pseudotumor (HIP) in the first case and a pancreatic neuroendocrine tumor (PNT) in the second (Fig. 1J–L). After administration of inhaled budesonin, resection of the PNT and initiation of phototherapy associated with a short course of prednisone (0.5mg/kg/day) for vitiligo, improve of the clinical picture and a reduction in the size of the liver lesion were observed.
OT is a rare entity, characterized by ossification and chondrification of the cartilages of the anterolateral tracheobronchial wall, without affecting the posterior wall, leading to the formation of submucosal nodules with bony/cartilaginous content, which protrude into the airway lumen.1 The fact that the nodules are easily visible on bronchoscopy makes this the diagnostic method of choice, since imaging tests can be indicative. Thus, radiography is usually normal in mild forms of the disease and tomographic findings (irregularity of the tracheal wall) can also be seen in infiltrative or granulomatous disease.1,2 Because of this, there are authors who consider histopathological study essential to establish the diagnosis, but the bony content of the nodules can make biopsy difficult.2
HIP is an infrequent lesion, and like OT, its etiology is unknown. Clinical and imaging findings are also nonspecific, and may be confused with neoplasms or metastatic lesions.3 It is theorized that an underlying inflammatory process (e.g., infections, autoimmunity) could be the cause behind both processes.4 In this specific case, it may be that the association of these three pathologies was the result of chance, but we can hypothesize that the history of autoimmunity, respiratory infections and the tumor process could justify the atypical association between OT and HIP.
Ethical ApprovalThe authors declare that the procedures followed conformed to the ethical standards of the responsible human experimentation committee and in accordance with the World Medical Association and the Declaration of Helsinki.
Informed ConsentThe authors have obtained the informed consent of the patients and/or subjects referred to in the article.
FundingThis research has not received any specific grants from agencies in the public, commercial or for-profit sectors.
Conflict of InterestsThe authors state that they have no conflict of interests.