Comorbidities are a fundamental part of managing patients with chronic obstructive pulmonary disease (COPD).1–3 The 2021 GesEPOC guide proposes classifying patients with COPD as low risk (LR) or high risk (HR) based on the degree of airflow obstruction, degree of dyspnea measured using the modified Medical Research Council (mMRC) scale and the history of exacerbations in the previous year.2 If we consider that each of these factors has been separately related to the existence of cardiovascular disease,4–8 it stands to reason that the sum of these increases the possibility of this type of comorbidity coexisting, which can impact the management of these patients. The aim of this study was to find the relationship between the summation of risk factors that make up the GesEPOC HR group and the coexistence of cardiovascular disease (CVD).
A cross-sectional, multicenter study was performed involving four historical cohorts of outpatients with COPD. These cohorts have been presented in previous studies.9 The following inclusion criteria were applied: (1) patient attending follow-up at an outpatient pneumology service; (2) age>40years; (3) active or former smoker with a pack-year index (PYI)≥10 or exposure to another known risk factor; (4) forced expiratory volume in one second (FEV1)/forced vital capacity (FVC) ratio<70% upon administration of 400μg of salbutamol. Chronic respiratory diseases other than COPD were considered an exclusion criterion except a history of asthma. Clinical data extraction was authorized by the corresponding ethics committee (Ethics Committee for Clinical Research of the University Hospital Nuestra Señora de Candelaria, registry number CHUNSC_2021_41).
Variables included were age, gender, body mass index (BMI [kg/m2]), pack-year index (PYI), dyspnea (mMRC scale) and the number of severe exacerbations requiring hospital stays during the year prior to the first visit as an outpatient. The comorbidities arterial hypertension (AHT), type 2 diabetes mellitus (DM2), dyslipidemia (DLP), obesity (defined as BMI≥30kg/m2), atrial fibrillation (AF), ischemic heart disease (IHD), chronic heart failure (CHF), cerebrovascular accidents (CVA), neoplasia (solid tumors, lymphoma, leukemia), osteoporosis, and mood disorders were obtained. Each associated morbidity was confirmed by a comprehensive review of the electronic medical records, data from diagnostic procedures, and disease-specific therapies. For the analysis, cardiovascular disease was defined as the presence of AF, IHD, CHF and/or CVA. The non age-adjusted Charlson comorbidity index (CCI) score10 and the BODEx11 index were determined for each patient. Forced spirometry data following bronchodilation was recorded. Patients were also classified as LR vs HR patients.2
For continuous normal variables, bivariate comparisons between independent samples were made using Student's t test. The Mann–Whitney U test was used for continuous non-normal variables. Qualitative variables were tested using Chi-square.
To study the association between the coexistence of CVD and the summation of the 3 risk factors, a multivariate logistic regression was performed with two models: model 1, which was adjusted for age, sex, BMI and PYI, and model 2 which, in addition to the previous adjustments, was adjusted for the existence of AHT, DM2 and dyslipidemia. In addition, the multiplicative effect of the combination of more than one risk factor including the interaction between risk factors and their main factors was evaluated; no interactions were significant. The model was not included in the results since it did not contribute to the interpretation of the simpler model. A p-value<0.05 was considered statistically significant. Analyses were performed using SPSS v.21 software.
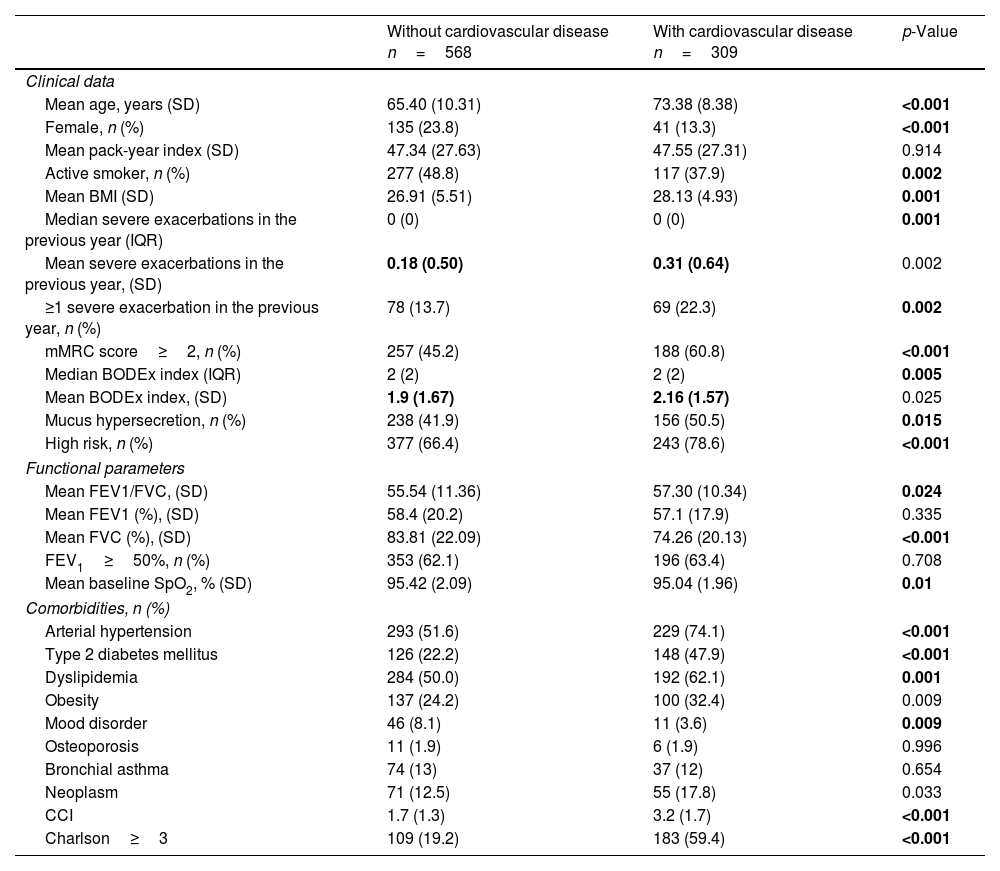
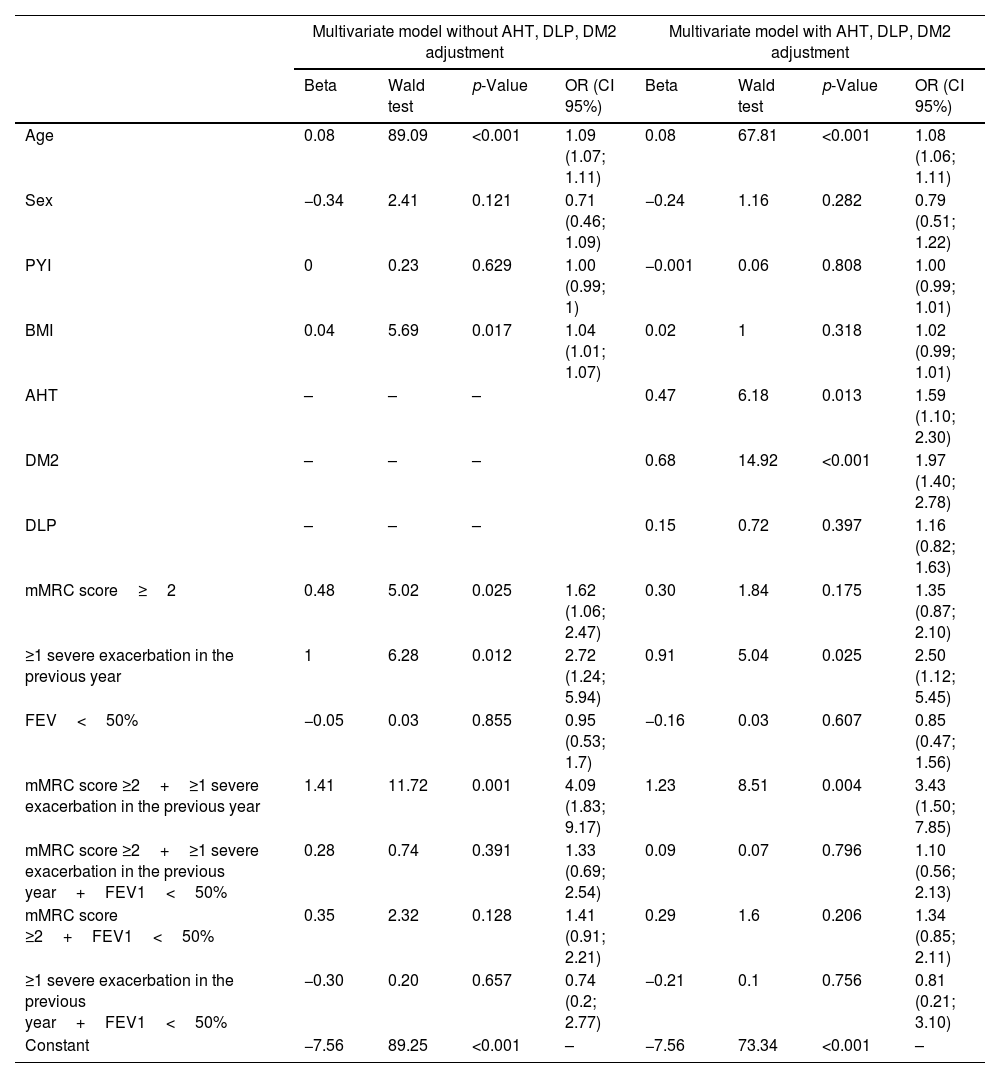
The baseline characteristics of the 877 patients comprising the study population have been presented in previous studies9 (70% were classified HR). The subjects with cardiovascular disease are described in Table 1. In the multivariate analysis (model 1), patients with dyspnea mMRC≥2 and those with a history of severe exacerbations in the previous year had a greater probability of coexisting cardiovascular disease (OR=1.62; CI95% 1.06–2.47; p=0.025 and OR=2.72; CI95% 1.24–5.94; p=0.012, respectively). The combination of these risk factors in a single patient independently increased the OR to 4.09 (CI95% 1.83; 9.17; p=0.001). 65% (CI95% 47.5–80%) of patients with both risk factors had CVD compared to 27% (CI95% 21.8–32.2%) of those without any risk factors. FEV1 was not significant when present on its own or in combination with the other risk factors. Age and BMI were associated with a greater likelihood of having cardiovascular disease (OR=1.08; CI95% 1.07–1.11; p<0.001 and OR=1.03; CI95% 1.01–1.07; p=0.017, respectively), Table 2.
Characteristics of patients with chronic obstructive pulmonary disease based on the presence of cardiovascular disease.
| Without cardiovascular disease n=568 | With cardiovascular disease n=309 | p-Value | |
|---|---|---|---|
| Clinical data | |||
| Mean age, years (SD) | 65.40 (10.31) | 73.38 (8.38) | <0.001 |
| Female, n (%) | 135 (23.8) | 41 (13.3) | <0.001 |
| Mean pack-year index (SD) | 47.34 (27.63) | 47.55 (27.31) | 0.914 |
| Active smoker, n (%) | 277 (48.8) | 117 (37.9) | 0.002 |
| Mean BMI (SD) | 26.91 (5.51) | 28.13 (4.93) | 0.001 |
| Median severe exacerbations in the previous year (IQR) | 0 (0) | 0 (0) | 0.001 |
| Mean severe exacerbations in the previous year, (SD) | 0.18 (0.50) | 0.31 (0.64) | 0.002 |
| ≥1 severe exacerbation in the previous year, n (%) | 78 (13.7) | 69 (22.3) | 0.002 |
| mMRC score≥2, n (%) | 257 (45.2) | 188 (60.8) | <0.001 |
| Median BODEx index (IQR) | 2 (2) | 2 (2) | 0.005 |
| Mean BODEx index, (SD) | 1.9 (1.67) | 2.16 (1.57) | 0.025 |
| Mucus hypersecretion, n (%) | 238 (41.9) | 156 (50.5) | 0.015 |
| High risk, n (%) | 377 (66.4) | 243 (78.6) | <0.001 |
| Functional parameters | |||
| Mean FEV1/FVC, (SD) | 55.54 (11.36) | 57.30 (10.34) | 0.024 |
| Mean FEV1 (%), (SD) | 58.4 (20.2) | 57.1 (17.9) | 0.335 |
| Mean FVC (%), (SD) | 83.81 (22.09) | 74.26 (20.13) | <0.001 |
| FEV1≥50%, n (%) | 353 (62.1) | 196 (63.4) | 0.708 |
| Mean baseline SpO2, % (SD) | 95.42 (2.09) | 95.04 (1.96) | 0.01 |
| Comorbidities, n (%) | |||
| Arterial hypertension | 293 (51.6) | 229 (74.1) | <0.001 |
| Type 2 diabetes mellitus | 126 (22.2) | 148 (47.9) | <0.001 |
| Dyslipidemia | 284 (50.0) | 192 (62.1) | 0.001 |
| Obesity | 137 (24.2) | 100 (32.4) | 0.009 |
| Mood disorder | 46 (8.1) | 11 (3.6) | 0.009 |
| Osteoporosis | 11 (1.9) | 6 (1.9) | 0.996 |
| Bronchial asthma | 74 (13) | 37 (12) | 0.654 |
| Neoplasm | 71 (12.5) | 55 (17.8) | 0.033 |
| CCI | 1.7 (1.3) | 3.2 (1.7) | <0.001 |
| Charlson≥3 | 109 (19.2) | 183 (59.4) | <0.001 |
Abbreviations: BMI, body mass index; FEV1, forced expiratory volume in 1s; FVC, forced vital capacity; CCI, Charlson comorbidity index score, not age-adjusted; mMRC, modified Medical Research Council scale; IQR, interquartile range.
Multivariate analysis of risk of coexistence of cardiovascular disease and summation of GesEPOC risk factors.
| Multivariate model without AHT, DLP, DM2 adjustment | Multivariate model with AHT, DLP, DM2 adjustment | |||||||
|---|---|---|---|---|---|---|---|---|
| Beta | Wald test | p-Value | OR (CI 95%) | Beta | Wald test | p-Value | OR (CI 95%) | |
| Age | 0.08 | 89.09 | <0.001 | 1.09 (1.07; 1.11) | 0.08 | 67.81 | <0.001 | 1.08 (1.06; 1.11) |
| Sex | −0.34 | 2.41 | 0.121 | 0.71 (0.46; 1.09) | −0.24 | 1.16 | 0.282 | 0.79 (0.51; 1.22) |
| PYI | 0 | 0.23 | 0.629 | 1.00 (0.99; 1) | −0.001 | 0.06 | 0.808 | 1.00 (0.99; 1.01) |
| BMI | 0.04 | 5.69 | 0.017 | 1.04 (1.01; 1.07) | 0.02 | 1 | 0.318 | 1.02 (0.99; 1.01) |
| AHT | – | – | – | 0.47 | 6.18 | 0.013 | 1.59 (1.10; 2.30) | |
| DM2 | – | – | – | 0.68 | 14.92 | <0.001 | 1.97 (1.40; 2.78) | |
| DLP | – | – | – | 0.15 | 0.72 | 0.397 | 1.16 (0.82; 1.63) | |
| mMRC score≥2 | 0.48 | 5.02 | 0.025 | 1.62 (1.06; 2.47) | 0.30 | 1.84 | 0.175 | 1.35 (0.87; 2.10) |
| ≥1 severe exacerbation in the previous year | 1 | 6.28 | 0.012 | 2.72 (1.24; 5.94) | 0.91 | 5.04 | 0.025 | 2.50 (1.12; 5.45) |
| FEV<50% | −0.05 | 0.03 | 0.855 | 0.95 (0.53; 1.7) | −0.16 | 0.03 | 0.607 | 0.85 (0.47; 1.56) |
| mMRC score ≥2+≥1 severe exacerbation in the previous year | 1.41 | 11.72 | 0.001 | 4.09 (1.83; 9.17) | 1.23 | 8.51 | 0.004 | 3.43 (1.50; 7.85) |
| mMRC score ≥2+≥1 severe exacerbation in the previous year+FEV1<50% | 0.28 | 0.74 | 0.391 | 1.33 (0.69; 2.54) | 0.09 | 0.07 | 0.796 | 1.10 (0.56; 2.13) |
| mMRC score ≥2+FEV1<50% | 0.35 | 2.32 | 0.128 | 1.41 (0.91; 2.21) | 0.29 | 1.6 | 0.206 | 1.34 (0.85; 2.11) |
| ≥1 severe exacerbation in the previous year+FEV1<50% | −0.30 | 0.20 | 0.657 | 0.74 (0.2; 2.77) | −0.21 | 0.1 | 0.756 | 0.81 (0.21; 3.10) |
| Constant | −7.56 | 89.25 | <0.001 | – | −7.56 | 73.34 | <0.001 | – |
Abbreviations: AHT, arterial hypertension; BMI, body mass index; DLP, dyslipidemia; FEV1, forced expiratory volume in 1s; mMRC, modified Medical Research Council scale; IQR, interquartile range. PYI, pack-year index; DM2, type 2 diabetes mellitus.
Similarly to model 1, after adjusting for the existence of AHT, DLP and DM2 (model 2), the risk of CVD coexistence was greater in those patients with a combination of a greater degree of dyspnea and a history of severe exacerbations, compared to the risk obtained with each of the GesEPOC risk factors separately. Subjects with a high degree of dyspnea showed an elevated risk of coexisting CVD, although it was not statistically significant, Table 2.
CVD is especially relevant, producing great morbidity and mortality.12–17 The GesEPOC risk classification was designed to guide the pharmacological treatment of COPD, but two of the classifying elements (dyspnea and exacerbations) can be conditioned by the existence of CVD.4,17 Therefore, using these elements just to decide on specific COPD therapies (e.g.: bronchodilators, steroids) may not be enough to improve patients’ quality of life and prognosis. Our hypothesis was that the presence of GesEPOC risk factors, particularly the sum of several of them, would be related to a greater prevalence of CVD. The results of the study confirm said hypothesis and show that the combination of a higher degree of dyspnea and a history of severe exacerbations is associated with a significantly higher prevalence of established CVD, even when adjusting for the classic cardiovascular risk factors. The practical implications of these results are clear: in patients classified as HR according to GesEPOC, and particularly those in which the two mentioned factors coincide, special attention must be paid to actively looking for CVD if we want to achieve the aim of optimal clinical control and reducing future risk.
It must be noted that we did not find any significant relationship between worse lung function and a greater prevalence of CVD. In this respect, there are conflicting previous results and although some studies agree with ours,18,6 others find an association between worse lung function and an increased risk of suffering these comorbidities.19
This study has several strengths, such as its multicentric nature and sample size. Its limitations include a potential information bias due to obtaining the study variables from the patients’ medical records, the cross-sectional nature of the study and the fact that the number of exacerbations treated on an outpatient basis was not recorded. Furthermore, the study population includes patients from pneumology clinics (70% HR) which partly limits the extrapolation of these results to other settings such as Primary Care clinics. On the other hand, given the characteristics of the study, we cannot rule out the existence of undiagnosed CVD that could influence our results, especially in those subjects with greater dyspnea and cardiovascular risk factors like DM2 or AHT, which would justify the results obtained in these subjects in model 2 of the multivariate analysis.
To conclude, high-risk patients according to GesEPOC must be carefully evaluated in order to rule out CVD if we want to achieve the objective of optimal clinical control and reducing future risk.
Authors’ contributionAll authors have made substantial contributions to the intellectual content and manuscript design and drafting.
ApprovalAll authors gave their approval to the final version of the manuscript and declare to have met the requirements for authorship.
FundingNo financial support has been received for conducting the study or drafting the manuscript.
Conflict of interestThe authors declare not to have any direct or indirect conflict of interest related to the manuscript contents.
Manuscript contents have not been submitted to or published previously in any other journal.