Although the evidence is still limited, studies describing the course of SARS-COV-2 infection suggest that the disease is mild in children. Most frequent complication is pneumonia, which occurs between 30 and 80% of cases, eventually requiring hospitalization.1–3 Pulmonary involvement has been described in children and adults in pauci or even asymptomatic patients, especially when computerized tomography (CT) is used. In fact, the sensitivity of CT has been suggested to be even higher than PCR for COVID-19 diagnosis, but is not justified in children.4
In recent years, point-of-care ultrasound (POCUS) is being increasingly used in pediatrics, as it is rapid, portable, repeatable, and non-ionizing. Specific patterns of lung ultrasound (LU) have shown to be useful in the differential diagnosis of pneumonia or acute bronchiolitis, with potential for prognosis.5–7 First case series describing main ultrasound findings in children with confirmed COVID-19 pneumonia have been published recently, suggesting a pulmonary involvement similar to the one described in other viral infections.8
The aim of this study was to address the usefulness of point-of-care LU, performed by pediatricians, to address pulmonary involvement in children with symptoms considered possibly attributable to SARS-CoV-2, during the first pandemic wave in Madrid.
We performed a prospective observational cohort study, including patients that consulted with symptoms attributable to SARS-CoV-2 infection, from April to June 2020 at the Paediatrics Department of a tertiary hospital in Madrid. The study protocol was reviewed and accepted by the local Ethics Committee.
Patients below 18 years of age evaluated for fever and/or respiratory symptoms were eligible for inclusion in the study. Exclusion criteria were: chronic lung disease, congenital heart disease, immunodeficiency, and congenital or anatomical defects of the airway.
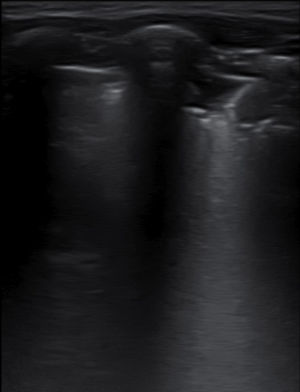
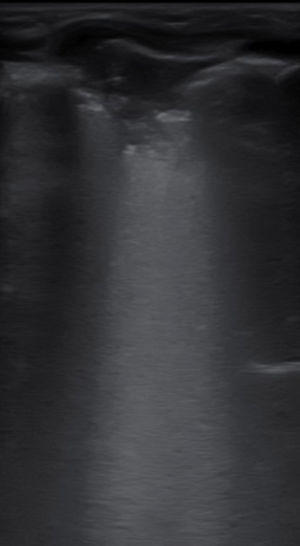
A LU was performed at the Emergency Room or within the first 24h of admission, using an E-Cube I7 (Alpinion Medical Equipment) equipped with a 3–12Hz lineal probe. Scans were performed by 4 pediatricians with ultrasonography experience, following a common systematic methodology including longitudinal and transversal sections collected on the anterior, lateral, and posterior chest wall, as previously described by Copetti et al.9 Ultrasound findings included: lung sliding, more than 3 B-lines per intercostal space, confluent B-lines and subpleural consolidations. The presence of A lines and fewer than 3 B lines per intercostal space defined normality.
All patients were managed according to the current treatment protocol. Data were collected from the patients’ medical records including all microbiological results, treatment and clinical outcome.
A total of 20 patients were included in this pilot study, with a median age of 5.2 years [IQR: 2.9–11.4], 65% were male. All patients were symptomatic, presenting with fever (80%), cough (55%), short of breathing (40%) and 45% were admitted for a median of 4.5 days [IQR:4–10]. Median duration of symptoms was 5 days [IQR: 2.5–8.5] and 25% of all patients needed oxygen support. SARS-CoV-2 infection was confirmed in 50% of patients either by PCR (42%) or by a positive serology (8%). In two cases, an alternate etiology was found (one mycoplasma, one metapneumovirus). No differences were found in epidemiological and clinical variables between COVID-19 confirmed and unconfirmed cases. Three cases (15%) were transferred to PICU without fatalities.
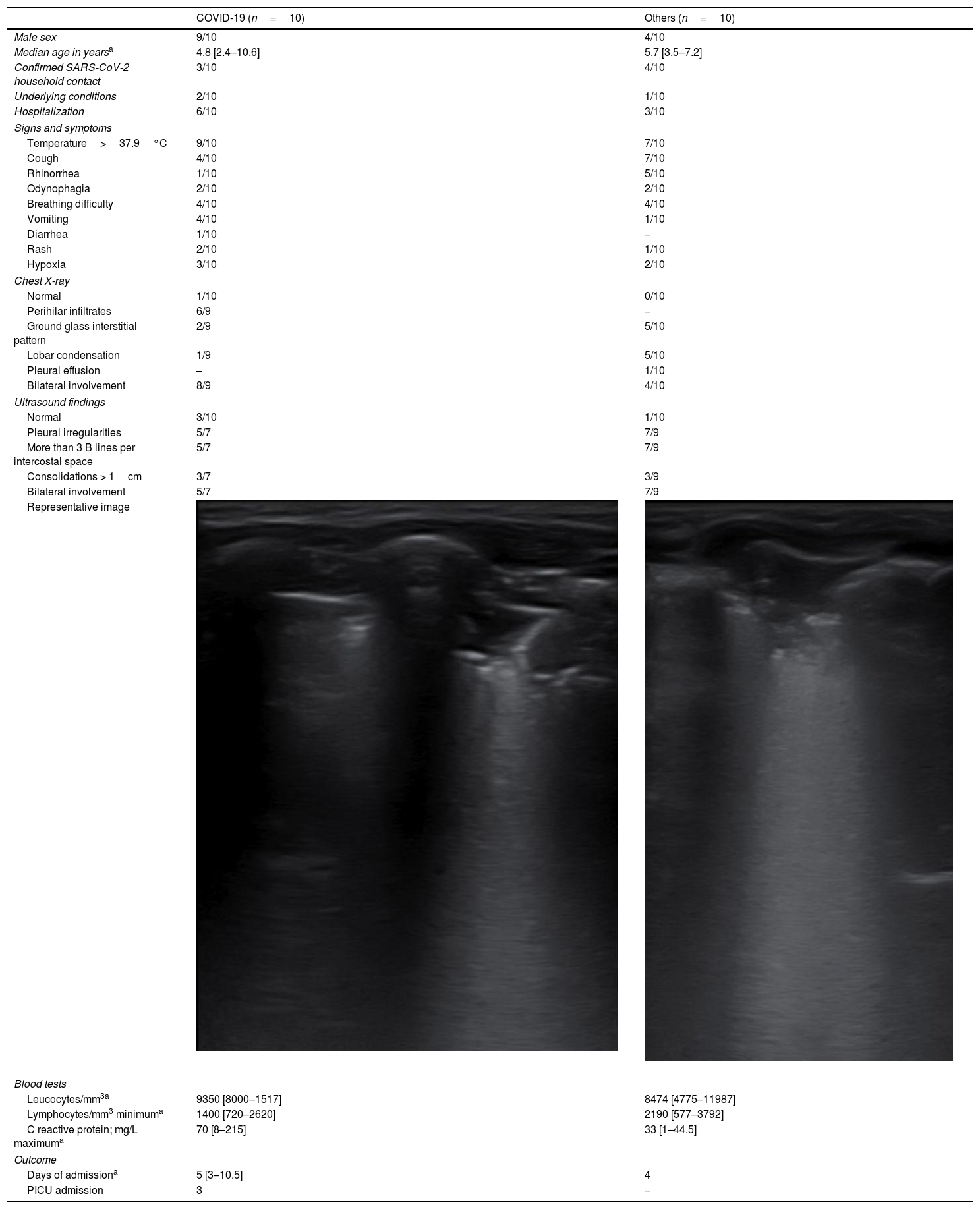
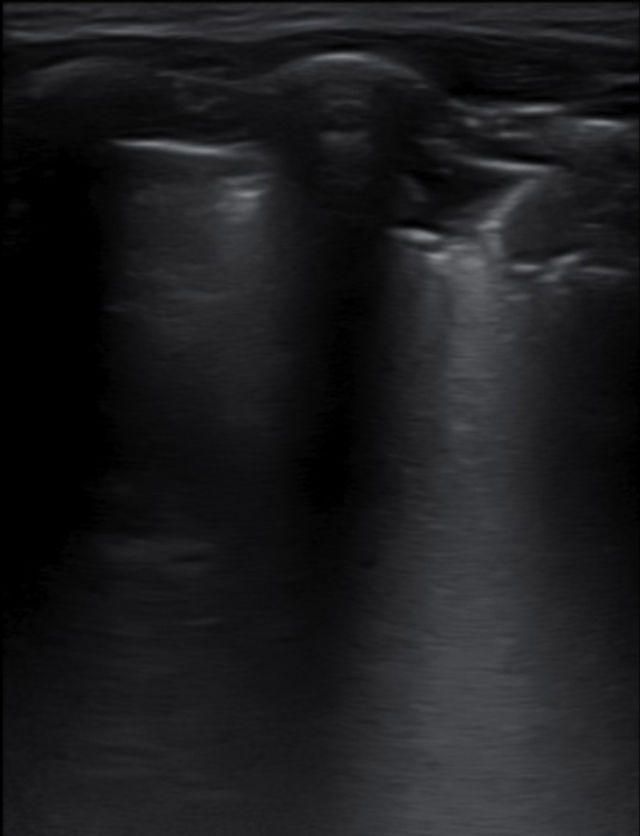
All but one patient had abnormalities on the chest X-ray, mostly ground glass opacities (35%), perihilar infiltrates (30%) and consolidations (30%), with no differences between the groups (Table 1). Three COVID-19 patients displayed a completely normal LU, vs. one in the comparison group. In all cases presenting with respiratory symptoms, LU revealed signs of lung involvement during COVID-19 infection. Ultrasound abnormalities were bilateral in 75% of cases in both groups. Pleural irregularities (50% anterior, 70% posterior), more than 3 B lines per intercostal space (uni or bilaterally) were present in 70% of cases, and consolidations in 30%, with no differences between groups. In total, six patients presented with consolidation bigger that 2cm (three in each group). There was no pleural effusion in any. The presence of ultrasound abnormalities did not predict the need of supportive oxygen. Isolated, none of the ultrasound findings showed high sensitivity for COVID-19, and no particular ultrasound pattern characterized the infection.
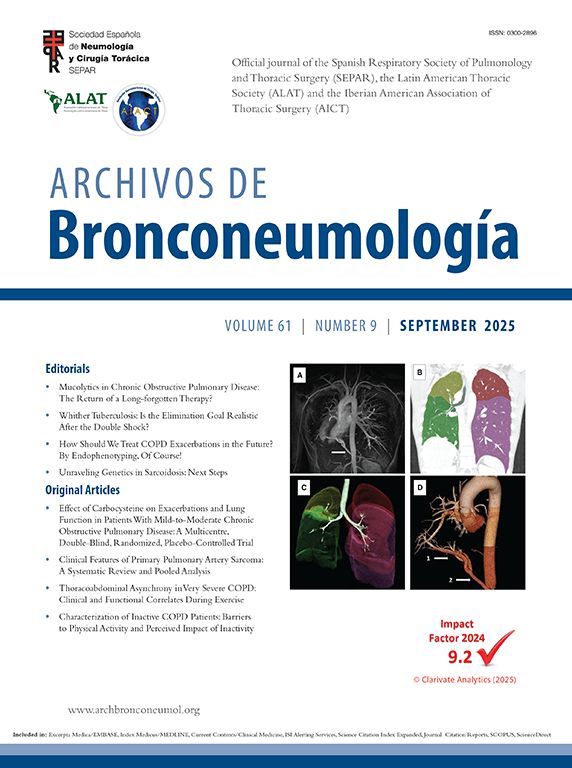
Clinical characteristics and lung ultrasound results in children with COVID-19 vs other respiratory infections.
| COVID-19 (n=10) | Others (n=10) | |
|---|---|---|
| Male sex | 9/10 | 4/10 |
| Median age in yearsa | 4.8 [2.4–10.6] | 5.7 [3.5–7.2] |
| Confirmed SARS-CoV-2 household contact | 3/10 | 4/10 |
| Underlying conditions | 2/10 | 1/10 |
| Hospitalization | 6/10 | 3/10 |
| Signs and symptoms | ||
| Temperature>37.9°C | 9/10 | 7/10 |
| Cough | 4/10 | 7/10 |
| Rhinorrhea | 1/10 | 5/10 |
| Odynophagia | 2/10 | 2/10 |
| Breathing difficulty | 4/10 | 4/10 |
| Vomiting | 4/10 | 1/10 |
| Diarrhea | 1/10 | – |
| Rash | 2/10 | 1/10 |
| Hypoxia | 3/10 | 2/10 |
| Chest X-ray | ||
| Normal | 1/10 | 0/10 |
| Perihilar infiltrates | 6/9 | – |
| Ground glass interstitial pattern | 2/9 | 5/10 |
| Lobar condensation | 1/9 | 5/10 |
| Pleural effusion | – | 1/10 |
| Bilateral involvement | 8/9 | 4/10 |
| Ultrasound findings | ||
| Normal | 3/10 | 1/10 |
| Pleural irregularities | 5/7 | 7/9 |
| More than 3 B lines per intercostal space | 5/7 | 7/9 |
| Consolidations > 1cm | 3/7 | 3/9 |
| Bilateral involvement | 5/7 | 7/9 |
| Representative image | ||
| Blood tests | ||
| Leucocytes/mm3a | 9350 [8000–1517] | 8474 [4775–11987] |
| Lymphocytes/mm3 minimuma | 1400 [720–2620] | 2190 [577–3792] |
| C reactive protein; mg/L maximuma | 70 [8–215] | 33 [1–44.5] |
| Outcome | ||
| Days of admissiona | 5 [3–10.5] | 4 |
| PICU admission | 3 | – |
Abbreviations: IQR, interquartile range; PICU, pediatric intensive care unit.
In this pilot study in children screened with COVID-19 suspicion, ultrasound findings on admission did not show predictive ability for the identification of SARS-CoV-2 infection. The accuracy of point-of-care thorax ultrasound was comparable to chest X-ray in order to detect lung abnormalities in the context of SARS-Co-V infection, but findings were indistinguishable from other respiratory infections.
The accuracy of PCR for the diagnosis of SARS-Co-V infection seems to be lower in children compared to adult patients.10 Chest X-ray is unspecific in most cases, and point of care ultrasound has been suggested as a promising tool by some pediatric studies.8 The accuracy of LU in detecting pediatric pneumonia of any etiology has been extensively proven,5,9,11 and the scarce data in the literature suggest that the accuracy in the context of COVID-19 is comparable.8 Main COVID-19 findings include pleural irregularities, vertical artifacts, areas of white lung and subpleural consolidations; all characteristic findings in the context of other viral respiratory infections such as acute bronchiolitis.6,12 Results of our study support these findings, with no abnormalities characterizing COVID-19. Although previous studies including infants admitted with acute bronchiolitis suggest that LU might help predicting clinical outcome, larger studies including severe cases of COVID-19 will be needed in order to test its role in patient stratification. In this context, the use of POCUS has aroused great interest among clinicians managing infected adults. In view of the recommendation of prono position to optimize ventilation of adults suffering from COVID-19, one could expect to find greater involvement when scanning the posterior wall, as described in acute bronchiolitis, where both B-lines and confluent B-lines are seen more often in the posterior area, but no differences were found in our series.
This is the first study that explores the usefulness of LU as a tool for identification of COVID-19 among children presenting with respiratory symptoms. Our study has several limitations, including the small sample size and the impossibility to completely exclude SARS-COV-2 infection and scans were not performed by a single person. Recruitment is ongoing to validate the usefulness of point of care ultrasound in children suffering from COVID-19.