Leptomeningeal carcinomatosis (LC) is a devasting complication for oncologic patients and the optimal therapeutic approach remains a challenge. Lung cancer is one of the most common primary tumors related with LC and Adenocarcinoma is the most frequent histological subtype involved.
We present the case of a 75-year-old man with a long history of smoking who was referred to our Hospital because of an abnormal nodule in the right lung detected by a routine chest radiology. A computed tomography (CT) scan showed a tumor of 30mm in the right upper lobe with no evidence of nodal involvement. The Positron Emission Tomography (PET) confirmed only glucose uptake by the tumor and there was no evidence of disease at the brain CT. A transthoracic CT-guided tumor biopsy was consistent with a primary adenocarcinoma of the lung. No mutations in epidermal growth factor gene or rearrangement in anaplastic lymphoma kinase were detected. An endobronchial ultrasound was performed with transbronchial needle aspiration of lymphadenopathies in 4R, 10R and 10L stations but pathological analyses were negative for cancer. Finally, a videomediastinoscopy showed evidence of Adenocarcinoma in one node of station 4R. Then, clinical stage III – A (cT2aN2M0) was established (8th Edition of the TNM Classification for Lung Cancer).
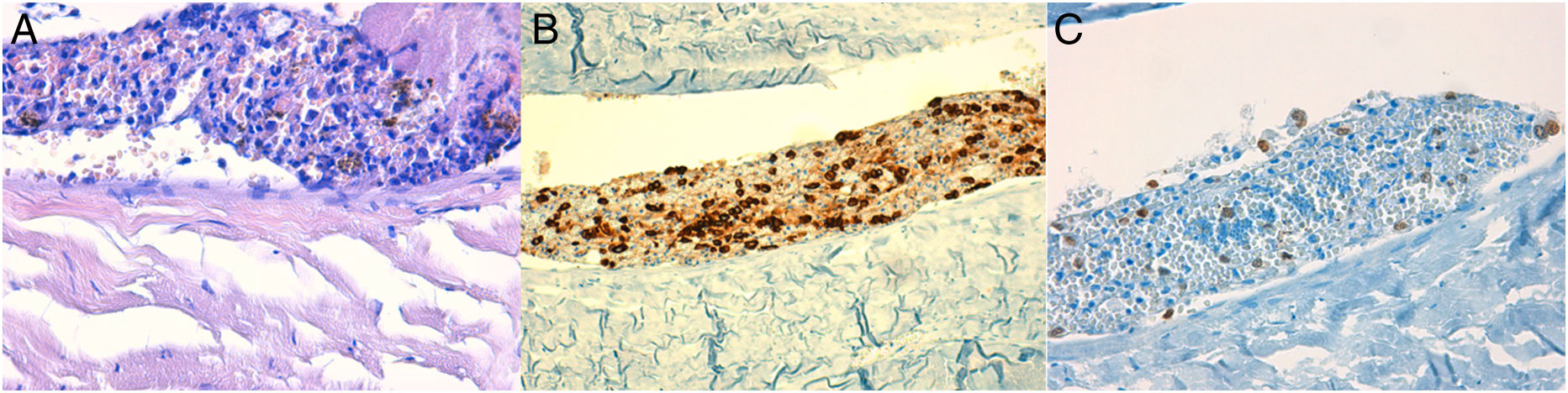
The patient presented an Eastern Cooperative Oncology Group performance status of 1 and treatment with chemotherapy and concomitant radiotherapy was planned. However, during the radiotherapy planning, the patient was admitted to our unit with a rapid clinical deterioration of the performance status and headache. The patient presented no fever or other symptomatology. In the physical examination only a mild instability to walk was detected. No papilledema. Presented normal values in serum calcium and ionogram. Blood cultures were negative. Magnetic resonance imaging (MRI) study of the central nervous system was completely normal. A lumbar puncture was performed twice with normal concentrations of glucose and proteins and no pathologic results in cytology and culture analysis of the cerebrospinal fluid. The patient presented progressive clinical worsening with deterioration of the level of consciousness and died after 11 days of hospitalization. An autopsy was performed showing evidence of isolated tumor cells of lung adenocarcinoma at the meninges (Fig. 1).
Histology of neoplasic cells at the meninge. (A) Epithelial proliferation in relation to meningeal tissue, cytologically formed by neoplastic cells of hyperchromatic small or medium size oval nuclei, with no apparent nucleolus and scarce cytoplasm. (Hematoxylin–eosin staining 40×.) (B) Cytokeratin AE1–AE3 positivity in the neoplastic cells. (Immunohistochemistry.) (C) TTF-1 focal positivity in the neoplastic cells. (Immunohistochemistry.)
In the present case we describe an atypical presentation of LC patient with a locally advanced lung adenocarcinoma and rapid clinical progression with neurologic impairment. No concise clinical diagnosis of LC or paraneoplastic syndrome could be made and patient died because of a rapid neurological deterioration. Finally, the autopsy was necessary for the diagnosed showing evidence of meningeal dissemination of the disease.
LC is a rare but rapidly fatal clinical condition found in approximately 5–8% of all patients with malignant solid tumors.1,2 In autopsy series, LC incidence may be 20% or more,3 suggesting that they are clinically underdiagnosed. Lung cancer is one of the most common primary tumors resulting in LC with an incidence of 4–9% among non-small cell lung cancer population, more frequent in adenocarcinoma subtype.2 The median survival time is only 4–6 months in selected patients who receive treatment and only 4–8 weeks in patients without treatment.5 Diagnosis is based on clinical, imaging and cerebral-spinal fluid (CSF) cytological examinations. MRI represent the gold standard for the imaging evaluation and LC involvement is observed in 40–75% of brain and in 15–25% of spine MRI. CSF evaluations are abnormal in more than 90%. However, in up to 30% of LC the CSF cytological analysis is negative.4 Thus, autopsy is sometimes necessary to get the diagnostic.
In conclusion, LC diagnosis can be a challenge and prognosis is still poor. Nowadays, some trials are being published reporting significant improvement of overall survival with new TKI and immunotherapy agents.3,5 A correct multidisciplinary management of the disease using those new therapies is a future challenge in cancer patients to improve the prognosis.