Schwannomas represent 5% of all tumours that can affect humans. At the respiratory level, intrapulmonary and intrabronchial schwannomas are extremely rare, account for 0.2% of lung neoplasms. Being the areas where this type of tumour is most frequently found are neck, cerebellar pontine angle, retroperitoneum and posterior mediastinum.1,2 We report the case of a patient with an intrapulmonary schwannoma.
Our patient was a 61-year-old male, active smoker of half a pack a day. He was referred by his primary care physician to the hospital for a study of constitutional syndrome and generalised arthromyalgia. Finally, he was diagnosed with polymyalgia rheumatica. However, during the process, a nodular retrocardiac image was observed by chance on the chest X-ray.
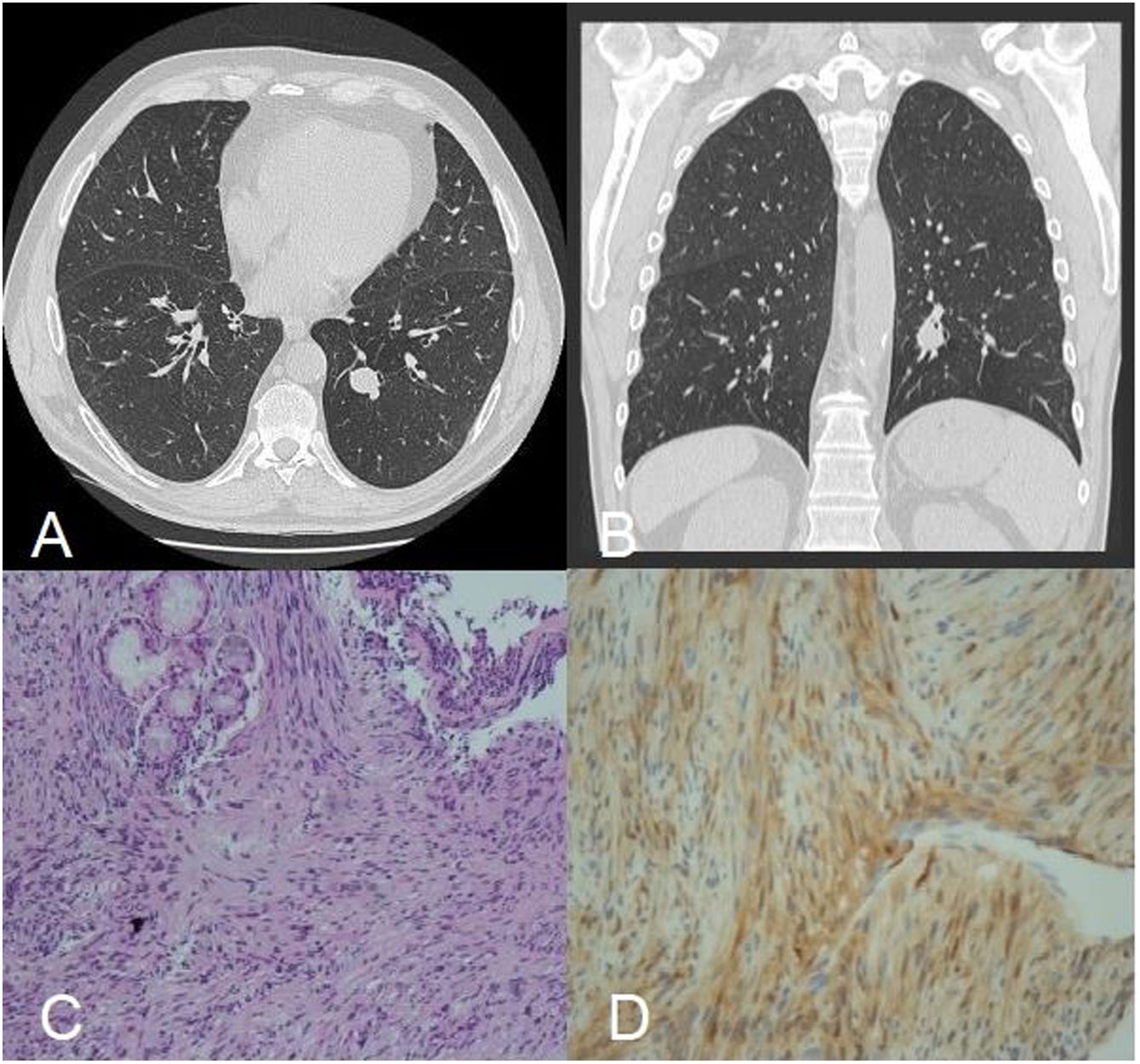
In view of this finding, a computed axial tomography (CT) scan of the thorax was performed, which confirmed the presence of a solitary pulmonary nodule measuring 2.2cm in the left lower lobe (LLL), with no evidence of other alterations (Fig. 1A, B).
(A, B) Computed axial tomography scan of the thorax, axial and coronal views showed a round, well delineated, 2.2cm nodule in the posterior segment of the left lower lobe. (C) Lung biopsy (haematoxylin and eosin stain; ×10) fusocellular and fasciculated stromal proliferation that traps pre-existing mucous-secretory glands. Characteristic histological features include cellular Antoni A. (D) Tumour cells were immunoreactive to S100.
Subsequently, a bronchoscopy was performed, showing only a partial stenosis of the bronchial lumen of the posterior segment of LLL.
Samples were sent to the pathology department, describing a bronchial mucosa occupied by a fusocellular and fasciculated stromal proliferation that traps pre-existing mucous-secretory glands inside and surround cartilaginous tissue (Fig. 1C). There was no atypia of significant mitotic activity, with minimal proliferative activity estimated with ki-67, around 1% of the cells. At the immunohistochemical level, they expressed only intensely and nuclear S-100 (protein found in cells derived from the neural crest, such as Schwann cells), being negative for Desmin, SMA, CD34, with non-valuable staining for CD10 (Fig. 1D).
For all these reasons, a diagnosis of intrapulmonary schwannoma was made. Finally, it was decided to proceed with surgical resection.
Intrapulmonary schwannomas occur asymptomatically and as a casual finding, producing different symptoms depending on the location and size, dyspnoea, cough, chest pain, and may even lead to the erroneous diagnosis of pneumonia or atelectasis. It is, therefore, important to make a good differential diagnosis.3
As in our case, the imaging test of choice for the characterisation of the neoplasm is a chest CT scan. After all, bronchoscopy is necessary for subsequent anatomopathological analysis to determine the specific treatment plan. In our case, the immunohistochemical analysis showed a ki67 of 1% and S100+, according to the benignity criteria for this type of neoplasm.2,4
For treatment, what has been found in the literature is the use of complete surgical resection, what was done in our case. There is evidence of few cases of recurrence, either by lobectomy or segmentectomy.2,5
Intrapulmonary schwannomas are an extremely rare tumour, where the characterisation of its epidemiology in a relevant way is still controversial due to the low incidence, especially in our environment. This case is relevant because, as far as we know, it is the first documented in the Iberian Peninsula, and the first in Europe after 8 years. In contrast with other continents, such as Asia, where the number of publications is higher.
FundingWe don’t have any source of funding.
Conflict of interestsThe authors state that they have no conflict of interests.