Tracheoesophageal fistulas (TEFs) secondary to the migration of an esophageal metallic stent are a serious yet infrequent complication, accounting for only 2% of all TEF cases.1 This complex condition, characterized by distinctive symptoms such as cough, dyspnea, malnutrition, and recurrent respiratory infections, significantly impacts patients’ prognosis, often leading to a life expectancy of 3–4 months.2
We present the case of a 51-year-old woman diagnosed in March 2023 with an infiltrating squamous cell carcinoma of the upper esophagus (cT4bN3M0) with a 13cm extension, 75% luminal stenosis, multiple lymph node involvement, and contact with the aorta, trachea, and bronchi without confirmed infiltration by bronchoscopy. The initial presentation included progressive dysphagia (initially for liquids, progressing to solid foods) and constitutional symptoms. The patient had an excellent baseline condition, ECOG 1, tolerated a pureed diet, and had a relevant history of active smoking (25 pack-years) and regular alcohol consumption (49g/day). A multidisciplinary committee decided on chemotherapy (CHT) and radiotherapy (RT) with curative intent due to the tumor's irresectability caused by lymph node metastases. The patient received five cycles of carboplatin–taxol and five sessions of radiotherapy at a dose of 180cGy each. A follow-up chest computed tomography (CT) revealed tumor progression with an increase in stenosis to 90%, and clinically, the patient developed aphagia. As a result, second-line treatment with folfox and nivolumab (PDL-1: TPS: 5% CPS: 7) was initiated, and a fully covered 2cm×8cm Taewoong esophageal stent was placed.
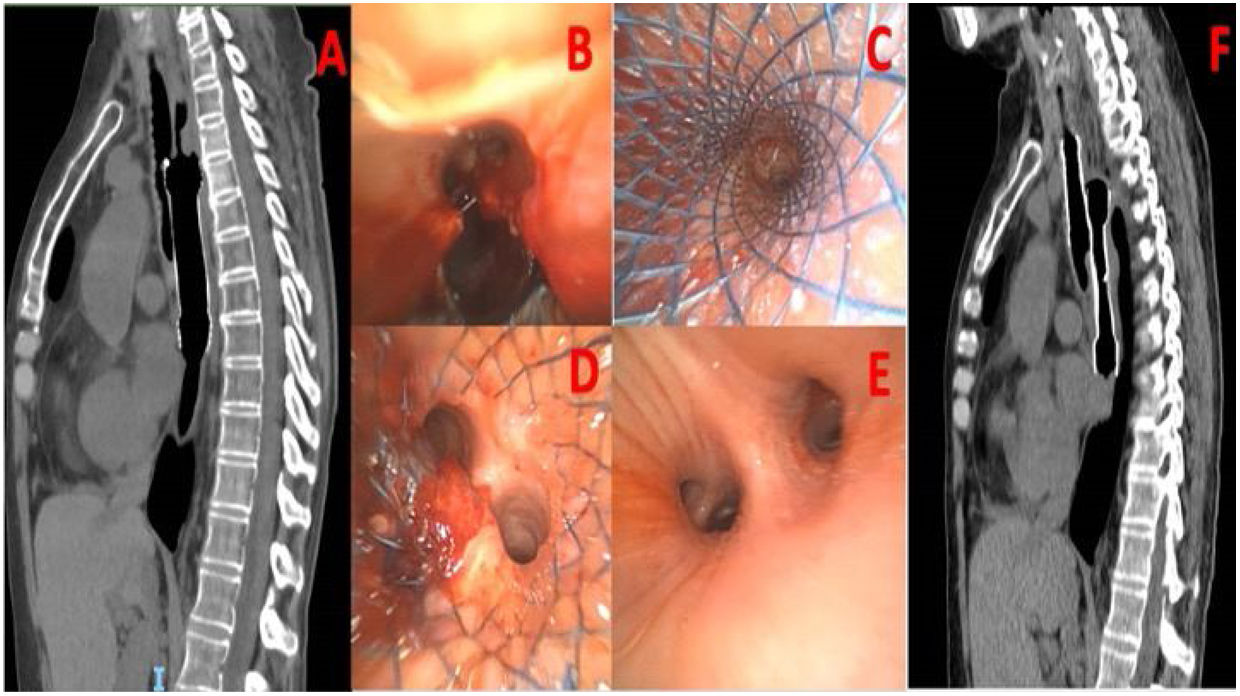
In November 2023, a reevaluation CT after three doses of the second line, with the patient asymptomatic and normal examination and laboratory tests, revealed a tracheoesophageal fistula (Fig. 1A), a diagnosis confirmed by bronchoscopy (Fig. 1B). After admission and the initiation of parenteral nutrition, the patient underwent rigid bronchoscopy, 48h later, in the operating room, resulting in the implantation of a self-expanding metallic tracheal prosthesis (Leufen aerstent TBS 2cm×5cm) (Fig. 1C). Despite the tracheal prosthesis, a fistulous hole persisted at the entrance to the left main bronchus (Fig. 1D). Therefore, the esophageal prosthesis was displaced cranially to overlap both prostheses, creating an “artificial wall” to completely close the fistula. Additionally, the integrity of the remaining left bronchial system was confirmed (Fig. 1E). In the immediate postoperative period, the patient experienced a fever spike, which did not result in any complications. Subsequent follow-ups demonstrated adequate oral tolerance, absence of dyspnea (0 mMRC), no episodes of respiratory infection, and proper positioning of both prostheses by chest CT (Fig. 1F).
(A) Chest computer tomography (CT): Tracheoesophageal fistula due to displacement of esophageal metallic prosthesis. (B) Bronchoscopy: Direct view of a large tracheoesophageal fistula extending from the trachea to the entrance of the left main bronchus. (C) Rigid Bronchoscopy: Placement of a self-expanding metallic tracheal prosthesis. (D) Rigid bronchoscopy: Persistence of the fistula despite the placement of the tracheal prosthesis. The esophageal prosthesis, visible on the left side, is decided to be displaced cranially. (E) Rigid bronchoscopy: Direct view of the intact left bronchial system. (F) Chest CT: Coronal visualization of both prostheses overlapped, forming an esophagotracheal artificial wall and sealing the fistula.
This outcome underscores the success of a multidisciplinary approach and innovative medical interventions in managing complex tracheoesophageal complications. It is crucial to note that bronchoscopy played a pivotal role in navigating and addressing the presented challenges.
AcronymsTEF: tracheoesophageal fistula; CHT: chemotherapy; RT: radiotherapy; CT: computed tomography.
Informed ConsentI confirm that I have obtained all consents required by applicable law for the publication of any personal details or images of patients, that are used in the materials submitted to Elsevier.
FundingThe authors state that no funding has been used for the elaboration of this manuscript.
Authors’ ContributionsAll authors have participated equally in the preparation of this article.
Conflicts of InterestThe authors declare no conflicts of interest.