The reason why there is a higher hospitalization rate due to asthma exacerbations amongst women is unclear. The objective of this study is to explore the possible causes that may explain this fact.
MethodsA multi-center, prospective study including asthma patients hospitalized in the pulmonary medicine departments during a 2-year period.
By means of a questionnaire, the following data were collected: demographic characteristics and treatment compliance, anxiety-depression, hyperventilation and asthma control, both prior to and during the hospitalization.
Results183 patients were included, 115 (62.84%) of whom were women. The women were older (52.4±18.3/43.4±18.7; P=.02), were more frequently prescribed inhaled corticosteroids (63.2%/47.1%; P=.03) and had a higher rate of hyperventilation syndrome (57.3/35.9; P=.02) and a longer mean hospital stay (7.3±3.4/5.9±3.6; P=.02). The percentage of smokers among the women was lower (21.2%/38.8%; P=.01) and the FEV1 was lower at admittance (58.2%±15.9%/67.5%±17.4%; P=.03).
In the 40–60-year-old age range, an association was demonstrated between being female and the ‘previous hospitalizations’ variable (OR, 16.1; 95% CI, 1.6–156.7); sex and obesity were also independently associated (OR, 4.8; 95% CI, 1.06–22).
ConclusionsIn this cohort, the rate of hospitalization for asthma was higher in women than in men. Being a woman between the ages of 40 and 60 is associated with previous hospitalizations and is a risk factor for asthma-related hospitalization. This situation could partially be explained by the hormonal changes during menopause, where polyposis and obesity are independent risk factors.
Las mujeres ingresan por exacerbaciones de asma con mayor porcentaje que los varones, sin que se conozcan claramente los motivos. El objetivo del estudio es explorar las posibles causas que expliquen este hecho.
Pacientes y métodosEstudio prospectivo multicéntrico en pacientes ingresados por asma durante 2 años en servicios de neumología.
Mediante cuestionario se recogieron: características demográficas, variables previas al ingreso y durante el mismo que incluían adherencia, ansiedad-depresión, hiperventilación, y control del asma.
ResultadosSe recogieron datos de 183 ingresos: 115 mujeres (62,84%). Las mujeres eran de mayor edad (52,4±18,3/43,4±18,7; p=0,02); había mayor porcentaje con prescripción de corticosteroides inhalados (63,2/47,1%; p=0,03) y síndrome de hiperventilación (57,3/35,9%; p=0,02), y una estancia media mayor (7,3±3,4/5,9±3,6; p=0,02). El porcentaje de fumadoras era menor (21,2/38,8%; p=0,01), y el FEV1 al ingreso era más bajo (58,2%±15,9/67,5%±17,4; p=0,03).
En el rango de 40 a 60 años se demostró una asociación entre ser mujer y la variable ingresos previos. De forma independiente, también se asociaron el sexo y la obesidad, con un OR de 16,1 (IC 95%, 1,6–156,7) y de 4,8 (IC 95%, 1,06–22), respectivamente.
ConclusionesEl porcentaje de ingresos por asma fue mayor en mujeres. Ser mujer entre 40 y 60 años se asocia con ingresos previos y constituye un factor de riesgo para ingreso por asma, en el que la hipótesis hormonal durante el climaterio podría explicar parte de los hechos. La poliposis y la obesidad son factores de riesgo, independientemente del sexo.
Despite the advances made in asthma management, this disease is still the cause of significant morbidity and mortality in adults.
The prevalence of childhood asthma is greater in males than in females (2:1, male:female), but this becomes progressively inverted after the age of 15.1–4
In children, the number of hospitalizations due to asthma among boys are double the number of hospitalizations in girls5–7 (2:1, under the age of 10), but the opposite is true among adults, when hospitalizations are more frequent among women.7–13
In 33269 hospitalizations due to asthma in 70 hospitals in the United States, Skobeloff et al.7 found that in the age group between 0 and 10, hospitalizations due to asthma was double in males than in females; conversely, three times more women were hospitalized between the ages of 20 and 50.
Similar data have been provided by other authors in different geographical areas and time-frames: in Denmark, in a longitudinal prospective study with a follow-up of 3540 people for 16 years, Prescott et al.8 saw that the women had a greater risk of hospitalization due to asthma than men, with an RR of 1.7. In England, Hyndman9 showed a progressive age-related increase in hospitalizations due to asthma in women. The same is true in Canada,10 although here the differences diminished among older patients. In a similar study, Trawick et al.11 report that the risk for hospitalization due to asthma in women versus men was 2.8 in the age range from 25 to 34. In more recent studies, Woods et al.12 and Lin et al.13 both reported that women between 18 and 45 were hospitalized 3.7 times more than men, and that the difference in hospitalizations due to asthma in women and men varied by age intervals, finding a maximum rate of 2.41 in the age range between 40 and 54.
In the autonomous community of Madrid, according to the data of the hospital morbidity survey and the CMBD database (Conjunto Mínimo Básico de Datos),14 the age-adjusted rates of hospitalization due to asthma by age were 76/100000 inhabitants for women and 58/100000 inhabitants for men. This differential data has held true since 1995.
Despite the differences in methodology and the quality of the studies, it seems to have been demonstrated that after a certain age there is a greater number of hospitalizations due to asthma in women, which is continuous although variable in the age range intervals.
The reasons for this predominance of women in hospitalizations due to asthma are not understood. Trawick et al.11 investigated the differences according to sex of those hospitalized with asthma, and they observed that women had an age 3.5 times higher than the men, but that there were no other differences in other variables, except that the males had a higher PCO2 upon admittance, which suggests a greater severity of the obstruction.
In the study by Woods,12 the women were also older and had more anxiety-depression, but there were no differences in obesity, ethnicity, smoking, gastroesophageal reflux, hypertension, diabetes, pneumonia or respiratory failure.
It seems reasonable to think that that one of the causes for more hospitalizations due to asthma is the severity of the crisis, although none of the studies have shown such data. Curiously enough, some published data are even contrary to this assumption.11
There are several theories that try to explain why women are hospitalized more than men in spite of a similar prevalence: greater disease severity as a consequence of hormonal mechanisms,15 differences in airway size,12 increased perception of obstruction in women,16 greater exposure and allergies to indoor allergens,16,17 or even less-than-optimal treatment due to the behavior of the patient and/or the physican18,19 or social inequalities.20 Seasonal variations do not seem to be related.21
Most studies are retrospective,9,10,13 and therefore the design is not adequate for determining the causes of the higher percentage of hospitalizations due to asthma in women. Understanding the causes of the increased hospitalizations could lead to better management of asthma patients and a decrease in hospitalizations, which would be accompanied by a savings in health expenses.
The objective of this study is to explore the possible causes that explain the current predominance of women in hospitalizations due to asthma.
Materials and MethodsStudy Design and PopulationA multicenter, prospective study with a selection of patients who had been hospitalized for asthma over the course of 2 consecutive years (March 2007–February 2009) in the pulmonology wards of six tertiary hospitals of the autonomous community of Madrid. Inclusion criteria for participation were: hospitalization due to asthma crisis, being diagnosed with asthma according to the American Thoracic Society criteria,22 age between 14 and 80. Exclusion criteria were: asthma patients hospitalized for causes other than asthma crisis, lack of collaboration or impossibility to perform the tests and age either less than 14 or over 80. The study was approved by the ethics committee (CEIC) of the Hospital Universitario Puerta de Hierro Majadahonda, and all the participants signed the corresponding informed consent.
ProcedureIn the patient data notebook designed for the study, the following data were systematically recorded: demographic characteristics, data prior to admittance (year of asthma diagnosis, work history, smoking, allergy studies [taking to be true a positive or documented reference to one or more allergens with skin-prick tests or in vitro reactivity for an aeroallergen]), comorbidities reported by the patient (rhinitis, psychiatric disease, gastroesophageal reflux, asthma treatment, number of crises, ER visits and hospitalizations due to asthma over the course of the previous 2 years), data of patient condition upon admittance (arterial blood gas and spirometry), as well as the time elapsed from the onset of the crisis to the arrival to the ER, considering an interval of 3 of more days to be late.
The Spanish versions of self-administered questionnaires within the first 72h were used to measure:
- •
Adherence, evaluated by six categorical-response questions (affirmation, negation) with regards to the 3 months prior to hospitalization: “Have you not carefully followed inhaler treatment on occasion?”; “Have you ever forgotten to use the inhaler?”; “Have you ever stopped using the inhalers because you felt better?”; “When you have felt better, have you ever used fewer inhalers or taken fewer puffs than prescribed by your doctor?”; “Have you ever stopped using the inhalers because you felt worse?”; “Have you ever used an inhaler other than what your physician prescribed because you felt you were having respiratory problems? (except rescue inhalers)”. The attitude towards treatment23–25 was considered compliant when the responses to all the questions posed were negative.
- •
Anxiety as a state and as a trait, assessed with the STAI inventory,26–28 which is designed to evaluate the transitory emotional condition (state) and anxiety as a trait (relatively stable propensity towards anxiety). Each of the positions is gauged by 20 items that receive between 0 and 3 points, and the total score ranges between 0 and 60 points. For this questionnaire, there are no proposed cut-points; instead, the scores that are obtained directly should be transformed into percentiles according to sex and age.
- •
Depression, assessed by the Beck questionnaire,29–32 with a score that ranges between 0 and 63 points, where the highest scores indicate a higher degree. A cut-point of 19 points adequately distinguishes between normality and moderate depression.
- •
Hyperventilation syndrome, evaluated with the Nijmegen questionnaire.33,34 It is made up of 16 items, with a graduated frequency between 0 and 4. A score equal to or higher than 23 is considered diagnostic for chronic hyperventilation syndrome,35,36 with a sensitivity and specificity of 91% and 96%, respectively.33
- •
Degree of control of the asthmatic disease according to the asthma control test (ACT),37,38 with a cut-point equal to or less than 15 to define poorly-controlled asthma.39
The data were input in a database (ACCESS 2000) and processed with a statistical software package (SPSS 14.0).
The association between sex and other factors were examined using Pearson's χ2 test to compare proportions and with the correction of continuity when the expected frequency was less than 5. To compare the continuous variables, the Student's t-test was used when the hypotheses for normality were met, and the nonparametric Mann–Whitney U when they were not. With a univariate analysis similar to that described, we tried to identify the variables associated with the severity of the patient upon hospitalization, as well as the estimation by age groups of the factors related with having previous hospitalizations and the comparison between women with and without previous hospitalization.
Later, a multiple logistic regression analysis was used to study the correlation of the “previous hospitalizations” variable and the variables that were significantly related in the univariate analysis in order to determine this association by age groups.
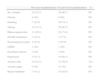
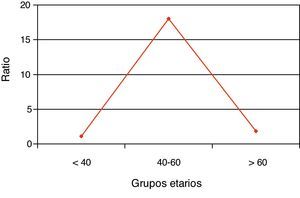
ResultsData were collected from 183 hospitalizations at six hospitals in Madrid. A total of 115 (62.84%) were women. The comparison between sexes is expressed in Table 1, showing among women an older age (52.4±18.3/43.4±18.7; P=.02), higher percentage of therapeutic prescription of inhaled corticoids (63.2%/47.1%; P=.03), longer mean hospital stay (7.3±3.4/5.9±3.6; P=.02), higher percentage of chronic hyperventilation syndrome (57.3/35.9; P=.02), lower percentage of smokers (21.2%/38.8%; P=.01), and a lower FEV1 upon hospitalization (58.2±15.9/67.5±17.4; P=.03).
Comparison by Sex of the Patients Hospitalized due to Asthma in Six Pulmonology Departments in Madrid.
| Males | Females | P | |
| Mean age, years | 43.4±18.7 | 52.4±18.3 | .002 |
| Asthma duration, years | 13.6±12.1 | 18.2±15.5 | .05 |
| Obesity (BMI>30) | 11 (27.5%) | 33 (34.4%) | NS |
| Smokers | 26 (38.8%) | 24 (21.2%) | .01 |
| Allergy | 35 (51.5%) | 59 (51.8%) | NS |
| Polyposis | 12 (17.9%) | 14 (12.4%) | |
| Rhinoconjunctivitis | 38 (56.7%) | 56 (49.6) | NS |
| Intolerance to NSAIDS | 13 (21.3%) | 25 (22.3%) | NS |
| GERD | 2 (3%) | 25 (22.1%) | .001 |
| Psychiatric disease | 4 (6%) | 15 (13.3%) | .1 |
| Previous hospitalizations | 20 (29.4%) | 46 (40.4%) | .1 |
| Treatment with IC | 32 (47.1%) | 72 (63.2%) | .03 |
| Self-treatment plan | 5 (8.2%) | 13 (13%) | NS |
| Delay (>72h) in going to ER | 26 (41.9%) | 59 (56.7%) | .046 |
| Sudden crisis (current) (≤3h) | 3 (4.8%) | 7 (6.7%) | NS |
| PCO2 | 39.8±10.5 | 38±8 | NS |
| FEV1, % | 67.5±17.4 | 58.2±15.9 | .03 |
| Mean stay, days | 5.9±3.6 | 7.3±3.4 | .02 |
| Poor control (ACT≤15) | 27 (73%) | 76 (75.2%) | NS |
| Depression | 13 (35.1%) | 44 (45.8%) | NS |
| Anxiety-state | 25.3±6.7 | 24.8±6.7 | NS |
| Anxiety-trait | 27.3±7.7 | 28.1±7.7 | NS |
| Good compliance | 8 (26.7%) | 30 (33.3%) | NS |
| Hyperventilation (≥23) | 14 (35.9%) | 55 (57.3%) | .02 |
BMI: body mass index; NSAIDs: non-steroid anti-inflammatory drugs; GERD: gastroesophageal reflux disease; ICS: inhaled corticosteroids; PCO2: partial pressure of carbon dioxide; FEV1: forced expiratory volume in 1s; ACT: asthma control test.
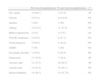
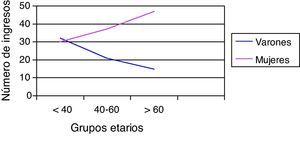
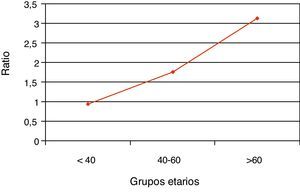
The percentage of hospitalizations prior to the current one in the last 2 years is higher in women, although without reaching statistical significance. By dividing the sample into tertiles, the number of hospitalizations increased with age only in women (Fig. 1), while the female/male ratio increased with age (Fig. 2). Nevertheless, the female/male ratio with previous hospitalizations other than the current one in the last 2 years reached its peak in the 40–60 age group (Fig. 3), where there was also a demonstrated association between being female and the number of previous hospitalizations.
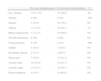
The results of the univariate analysis by age groups in order to determine the factors related with having previous hospitalizations (Tables 2–4) provided the following data: in the age group under 40, there was a significant association with the anxiety-state variable. In the 40–60-year-old age range, there was a demonstrated significant association with sex (female), obesity and nasal polyposis. In those over the age of 60, the association was significant with sex (male), rhinoconjuntivitis (as a protector factor) and with depression.
Factors Associated With Previous Hospitalizations in Patients Under the Age of 40.
| Previous hospitalizations | No previous hospitalizations | P | |
| Sex, females | 10 (32.3) | 20 (66.7) | NS |
| Obesity | 4 (40) | 6 (60) | NS |
| Smoking | 7 (25.9) | 20 (74.1) | NS |
| Allergy | 14 (33.3) | 28 (66.7) | NS |
| Rhinoconjunctivitis | 11 (28.2) | 28 (71.8) | NS |
| NSAID intolerance | 2 (22.2) | 7 (77.8) | NS |
| Nasal polyposis nasal | 4 (44.4) | 5 (55.6) | NS |
| GERD | 1 (50) | 1 (50) | NS |
| Psychiatric disease | 2 (50) | 2 (50) | NS |
| Depression | 5 (33.3) | 10 (66.7) | NS |
| Anxiety-state | 16 (43.2) | 21 (56.8) | .021 |
| Anxiety-range | 9 (30) | 21 (70) | NS |
| Hyperventilation | 7 (41.2) | 10 (58.8) | NS |
NSAID: non-steroid anti-inflammatory drugs; GERD: gastroesophageal reflux.
Factors Associated With Previous Hospitalizations in the 40–60-Year Age Range.
| Previous hospitalizations | No previous hospitalizations | P | |
| Sex, females | 19 (51.43) | 18 (48.6) | .00 |
| Obesity | 9 (60) | 6 (40) | .036 |
| Smoker | 5 (23.8) | 16 (76.2) | NS |
| Allergy | 11.(37.9) | 18 (62.1) | .18 |
| Rhinoconjunctivitis | 11 (31.4) | 24 (68.6) | NS |
| NSAID intolerance | 6 (40) | 9 (60) | NS |
| Nasal polyposis | 6 (75) | 2 (25) | .008 |
| GERD | 4 (36.4) | 7 (63.6) | NS |
| Psychiatric disease | 2 (33.3) | 4 (66.7) | NS |
| Depression | 7 (38.9) | 11 (61.1) | NS |
| Anxiety-state | 14 (38.9) | 22 (61.1) | NS |
| Anxiety-range | 12 (35.3) | 22 (64.7) | NS |
| Hyperventilation | 9 (39.1) | 14 (60.9) | NS |
NSAID: non-steroid anti-inflammatory drugs; GERD: gastroesophageal reflux.
Factors Associated With Previous Hospitalizations in Those Over the Age of 60.
| Previous hospitalizations | No previous hospitalizations | P | |
| Sex, males | 10 (66.7) | 5 (33.6) | .05 |
| Obesity | 9 (47.4) | 10 (52.6) | NS |
| Smoker | 1 (50) | 1 (50) | NS |
| Allergy | 12 (52.2) | 11 (47.8) | NS |
| Rhinoconjunctivitis | 5 (25) | 15 (75) | .02 |
| NSAID intolerance | 6 (42.9) | 8 (57.1) | NS |
| Nasal polyposis | 5 (55.6) | 4 (44.4) | NS |
| GERD | 7 (50) | 7 (50) | NS |
| Psychiatric disorder | 5 (55.6) | 4 (44.4) | NS |
| Depression | 17 (70.8) | 7 (29.2) | .00 |
| Anxiety-state | 12 (37.5) | 20 (62.5) | .09 |
| Anxiety-trait | 13 (41.9) | 18 (58.1) | NS |
| Hyperventilation | 14 (48.3) | 15 (51.78) | NS |
NSAID: non-steroid anti-inflammatory drugs; GERD: gastroesophageal reflux.
In the logistic regression analysis in the age group between 40 and 60, being female and obesity were the only two factors that were independently associated with having previous hospitalizations with OR of 16.1 (95% CI, 1.6–156.7) and 4.8 (95% CI, 1.06–22), respectively. In the age group over the age of 60, the only variable that was independently associated was depression, with an OR of 12.2 (95% CI, 2.7–54.2).
The univariate analysis comparing women with and without previous income showed a significant association between income with obesity or nasal polyposis, which are variables that are generally associated with this age range.
DiscussionThe analysis of the data of our study presents two different aspects: factors related with the current hospitalization due to asthma, and those that correlate with the history of previous hospitalizations in the previous 2 years.
In the current hospitalization, we confirmed a progressive increase in the female/male ratio by age groups, while the ratio with the history of previous hospitalizations in the last 2 years showed a very significant peak in the 40–60 age range, where being female was also an independent risk factor associated with previous hospitalizations.
Some papers have confirmed a higher number of hospitalizations due to asthma related with age.13 Meanwhile, in our study this circumstance only occurs in women, without being able to find a justification or similarity in the literature, aside from some aspects such as regional or climatic differences and differences among cities, or even that male asthma patients who smoke with chronic airflow limitation are identified as chronic obstructive pulmonary disease (COPD) given the existing overlapping between these two entities.
In the current hospitalization, there is a higher percentage of chronic hyperventilation in the hospitalized women, which could lead one to contemplate its influence on the higher number of hospitalizations. The higher percentage of women with anxiety and hyperventilation syndrome is reported in the literature.40 In asthmatics, the percentage is even greater, with a predominance in women.40,41 Some studies show that in people with asthma, especially in the severest forms, the presence of psychiatric disorders, especially those related with anxiety, is the cause of an increased use of health-care resources, including hospitalizations due to asthma.42,43 Nevertheless, the results obtained in our paper from the analysis of previous hospitalizations do not support this idea.
Furthermore, the hospitalized women are older, report a higher percentage of gastroesophageal reflux, take longer to seek emergency assistance, present with a state of greater severity and the average stay is longer, despite a smaller percentage of smokers and a proportionally greater inhaled corticosteroid use.
In some studies, no differences are found in pulmonary function44,45 or blood gases,46 even when the analysis is controlled for prevalence and smoking.47 The greater severity upon hospital admission could be explained by the delay in going to the ER, which could be a consequence of a greater number of visits to the primary care physician, or due to having a probability that is 5 times greater than in men of receiving treatment with oral corticosteroids in the same period of time.48 It cannot be determined whether this fact is due to a preferential medical tendency, whether it is a result of increased visits to the primary care physician or whether it is the result of an alteration in the perception of asthma symptoms, as women tend to be better treated, their treatments better follow the clinical practice guidelines,49 they use PEF monitors more regularly50 and more closely follow written self-care plans,50,51 even though there are reports to the contrary in the literature.52
The analysis of previous hospitalizations explains with greater resolve the idiosyncrasies of subjects with risk for hospitalization, without the incidental circumstances of seasonality or triggers that may have led to the current hospitalization.
Several studies have demonstrated that the factor that heavily contributes to being admitted is having had previous hospitalizations.53,54
The finding of a peak in the female/male ratio in the age range between 40 and 60 agrees with the results of other studies.4,10,13
In our study, being female is associated with previous hospitalizations, not only in the univariate analysis, but also in the multivariate, and also as an independent risk factor with obesity. This finding agrees with other studies55,56 showing that obesity is a risk factor for previous hospitalizations.
With regards to nasal polyposis, in our study there is an association with hospitalizations in the univariate analysis, a finding that coincides with the study by Ceylan et al.,57 a prospective study that found that the presence of nasal polyposis in subjects with asthma is associated with poorer asthma control and a greater number of ER visits and hospitalizations. The association between nasal polyposis and intolerance to non-steroid anti-inflammatory drugs has been reported in several studies associated with severity,58,59 although the contribution of each of these could not be determined in an isolated manner.
These data support the idea that it is mainly only factors implicit in being female that intervene in a higher risk for hospitalization. Hormonal influences have been related with asthma severity and the use of resources,60 and a correlation with menopause has been hypothesized.13,61–64 The age range between 40 and 60 generally encompasses the pre- and post-menopausal phases that correspond with this transitional time period in women, which is the consequence of ovarian depletion. Some studies indicate that substitutive hormone therapy increases the risk for asthma.65 In our case, this datum has not been collected and therefore cannot be analyzed.
The limitations of our study are a direct consequence of its design and may be present in any and all cross-sectional studies.
In this direction, there may be confounding factors related to exposure variables (trigger factors) that act as causal agents for risk and may lead to distortion of the effect variable (hospitalization). These can influence the results in any direction, mainly if there is an inhomogeneous distribution among the study groups, or if they have influenced in the sample selection, giving rise to false associations or concealing others that do exist. Moreover, many of the variables compiled that do not have an objective determination are subject to memory bias and have not been later verified, but there is the possibility that this may not have made a difference in the categorization of the individuals.
It is evident that there may be a certain element of selection bias by compiling only the hospital admissions that took place in the pulmonology departments, knowing that a certain number of hospitalizations take place in the internal medicine departments.
In conclusion, being female is a risk factor for hospitalization due to asthma only in the 40–60-year-old age range, where the hormonal hypothesis could justify this fact. Polyposis and obesity are risk factors, regardless of sex, in this same age range interval.
FundingThis study has been financed by Neumomadrid.
The authors would like to acknowledge Isabel Millán Santos, from the Biostatistics Department at the Hospital Universitario Puerta de Hierro Majadahonda, for her invaluable help in the statistical analysis.
Please cite this article as: Melero Moreno C, et al. Factores relacionados con el mayor porcentaje de ingresos por asma en mujeres. Estudio FRIAM. Arch Bronconeumol. 2012;48:234–9.