Dengue fever (DF) is a mosquito-borne tropical disease spread by female Aedes aegypti. Belonging to the Flavivirus family, it has 4 unique serotypes (DEN1-4). The incubation period for DF reaches upto 7 and 10 days. It is currently endemic in 128 countries, mostly developing countries, putting an estimated 3.97 billion population at risk each year. Clinical illness can range from asymptomatic DF to life-threatening dengue hemorrhagic fever (DHF) and dengue shock syndrome (DSS). DSS are related to worse outcomes in dengue patients. These severe clinical state manifests as a multi-organ failure involving the heart, brain, liver, lungs and kidneys.1,2 DF is mostly a self-limiting disease with comparatively low mortality; few characteristic features are fever with chills, myalgias, arthralgia, headache, retro-orbital pain, vomiting, and rash.2 However, there are many other rare yet serious manifestations that are observed in patients with DF which are labeled as expanded dengue syndrome (EDS) and its serious manifestations are labeled as DHF and DSS as mentioned above.3
As far our knowledge reaches, there is scarcity of research exploring the role of physiotherapy in pediatric population to overcome the cardio-respiratory comorbidities in child presented with EDS. Here we present a case of EDS with additional cardiorespiratory involvement.
Case ReportThe patient was a 7-year-old male child presented with fever, pain in abdomen, generalized body weakness and difficulty in breathing from past 3 days prior to the hospital admission. No previous respiratory pathologies, not relevant medical and surgical histories were noticed. Child was immunized as per age according to informant (mother). Patient belonged to lower middle class (score=12) of socioeconomic status according to modified Kuppuswamy scale which may influence the patient compliance in context of treatment. Child was stable with 5l of oxygen administered with nasal prongs when first time physiotherapy assessment was done. Child was using accessory muscles typically sternocleidomastoid and upper trapezius, supraclavicular retractions were observed in both the sides, along with non-pitting edema over both the ankles. Grade 2 tenderness was present over the right hypochondriac region of abdomen with generalized body weakness. Blood tests including complete blood count, renal and lever function tests have shown decreased hemoglobin levels, hematocrit (30.6%, normal value: 36–37%), and elevated total leukocyte count (14.51000/cumm, normal value: 4–101000/cumm), urea, uric acid levels, total bilirubin, serum glutamate pyruvic transaminase (SGPT: 244U/L, normal value: 5–35U/L) and serum glumate-oxaloacetic transaminase levels (SGOT: 1100.8U/L, normal value: 5–35U/L). Nonstructural protein 1 antigen test and Typhi DOT were positive. X-ray findings were more haziness in lower lobes with consolidation. To quantify the prognosis, chest expansion (centimeters), single breath count (count/breath), incentive spirometer [IS] (cm3/s) and WeeFIM was used. WeeFIM (ICC=>0.9), an 18-item instrument with a 7-level ordinal scale and total score of 126, helpful in assessing child's consistency in the performance of functional abilities. Self-care, mobility, and cognition are the three basic areas that are evaluated through interviews or by seeing a child performing a task in accordance with criteria.4
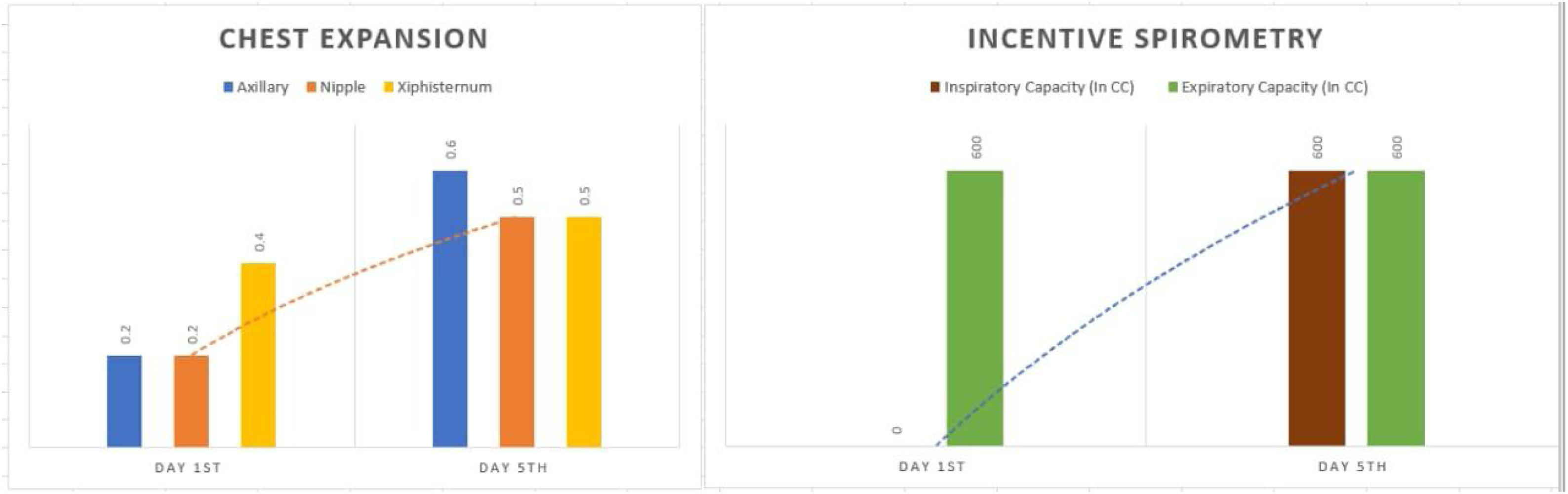
Goal directed physiotherapy intervention was administered to reduce edema, increase the chest expansion, enhance the proper use of respiratory muscles and maintain the quality of life on day 7 after admission. Readings of chest expansion were 1cm for axillary, 1cm for nipple and 1.7cm for xiphoid region on first day of physiotherapy assessment. Child was not able to initiate the inspiration (poor inspiration) and 600cc using incentive spirometry. Metronome is a mobile application which can be used to quantify the single breath count according to beats. Child counted only 6 beats in single breath hold, checked by metronome. Exercise regime was followed during stay in IPD settings. For effective use of respiratory muscles and chest expansion, active paced breathing, thoracic expansion exercises and diaphragmatic breathing was administered. WeeFIM score was 46 on day one. On fourth day as child was showing improvements in respiratory symptoms and walking abilities, we assessed functional mobility by performing 10 meters walk test (10mWT) in corridor area of IPD. Child was in recovery phase so we analyzed rate of perceived exertion after any physical activity by using modified Borg scale. Child maintained his oxygen saturation in room air (SPO2=96%). Child covered 10m in 15.67s with grade 4 on modified Borg scale (somewhat severe). Treatment started with the 2 sets active cycle of breathing technique, and static marching near bed side area. Previous treatment was also accounted on fourth day. The intervention was continued for one week. All the outcome measures were assessed on seventh day. On seventh day, lab reports showed improvements in hematocrit (34.6%, normal value: 36–37%) and total leukocyte count (12×1000/cumm, normal value: 4–10×1000/cumm) levels. Chest expansion was 2.5cm for axillary, 2.5cm for nipple and 2.7cm for xiphoid region. Child was able to perform the inspiration; 600cc and 600cc of expiration using IC (Fig. 1). WeeFIM score was 54. Child counted 12 beats in single breath measured with Metronome app.
Lung abnormalities are uncommon in dengue however there are possibilities of few systemic changes which can affect the functioning of lungs. Physiotherapy intervention may work as potential treatment adding with medical treatment for the reduction of symptoms. The child's active participation was also enhanced the recovery. This case reported positive effects of physiotherapy intervention in child with EDS.
FundingNone declared.
Ethical ApprovalThe case report was performed according to the principles laid by, declaration of Helsinki (Revised 2013), and National guidelines for biomedical and health research involving human participants (2017).
Conflict of InterestNone declared.