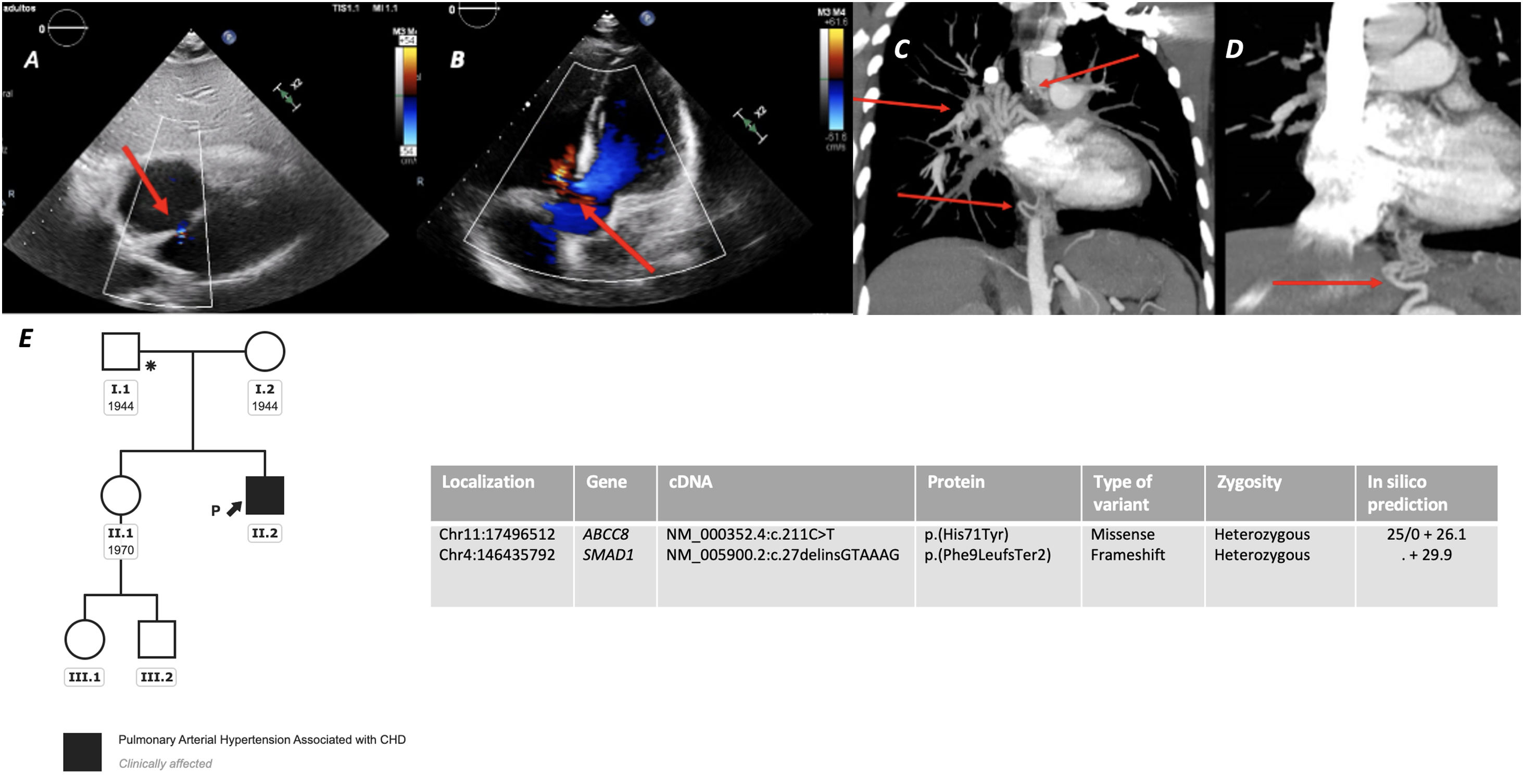
A 10-year-old male with progressive dyspnea was diagnosed of Pulmonary Arterial Hypertension (PAH) related to a small atrial septal defect (ASD) (Fig. 1, panel A) and a restrictive perimembranous ventricular septal defect (Fig. 1, panel B). The initial right heart catheterization demonstrated suprasystemic pulmonary artery pressure (138% of systemic pressures), right to left shunting (Qp/Qs 0.4), indexed pulmonary vascular resistance of 39Wood Units/m2, and a transpulmonary gradient of 76mmHg. On triple sequential therapy with Tadalafil, Macitentan and subcutaneous Treprostinil, a Lenus implantable pump for intravenous Treprostinil was implanted at his 26 years. At that time, oral anticoagulation was also introduced. Despite progressive dilatation of the right chambers and persistent suprasystemic pulmonary pressures, the patient remained in functional class II until 28, when he was admitted due to an episode of life-threatening hemoptysis. After stabilization, a pulmonary angiography and an angio-CT were done, in which multiple thoracic collaterals were noticed (Fig. 1, panels C and D). One bronchopulmonary collateral was actively bleeding, and an embolization was then performed. The patient responded favorably and was discharged, withdrawing Acenocoumarin. On maximum vasodilator therapy, without new hemoptysis episodes, the patient has remained at high-risk stratum. Nevertheless, considering the presence of multiple collaterals in the mediastinum and the pleura, the patient has recently been considered not candidate for bilateral lung transplantation or heart-lung transplantation at his 29 years of age.
Panel A. Incidental atrial septal defect detected in TTE, showing right-to-left shunting (red arrow); Panel B. Small perimembranous ventricular septal defect (VSD) with Left-to-right shunting during systole (red arrow); Panels C and D. Reconstruction of some of the thoracic collaterals noticed in the mediastinum in the angiographic computed tomography (red arrows); Panel E. Genetic analysis and segregation study of first-degree relatives.
Shortly after diagnosis, the index-case parents consented his inclusion in the Spanish Registry for pediatric pulmonary hypertension (REHIPED).1 A genetic test was performed when he was 28, as part of a research study in patients in that registry, revealing two significant variants among candidate genes related with the development of PAH (SMAD1 and ABCC8). Both variants were classified as likely pathogenic initially by the in vitro analysis.2 The evaluation of first-degree relatives revealed the presence of the SMAD1 variant in the 30-year-old asymptomatic sister and the father of the index case. This last individual underwent an ASD closure at the age of 30 due to right chambers dilatation. After the segregation studies, the variant was maintained as likely pathogenic. The ABCC8 was a rare de novo variant, not previously described in the literature, and not present in other first-degree relatives, which permitted in this case the reclassification of the variant as pathogenic (Fig. 1, panel E).
Genetic testing for PAH-associated candidate genes can be considered for patients with CHD and “out of proportion” PAH.3 The genetic background of such cases, in which the size of the defect unlikely explains the severity of vascular disease, should be taken into account, not only when shunt closure is considered or for genetic counseling, but also in the evaluation for lung transplantation. Certain mutations are associated with widespread collateral vessels.4 Specifically, SOX17 variants have been related with PAH-CHD, with high prevalence of thoracic collaterals.5 Although genetics have not demonstrated a prognostic value in PAH, the presence of gene variants could be associated with specific phenotypes and management implications, as demonstrated in this rare case with a digenic inheritance.
Author contributionSubstantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work: ACU, PES, JTC, MJC.
Drafting the work or revising it critically for important intellectual content: ACU, PES, JTC, MJC.
Final approval of the version to be published: ACU, PES, JTC, MJC.
Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: ACU, PES, JTC, MJC.
FundingThis project was funded by project “Bases Genético-Moleculares de la Medicina de Precisión en la Hipertensión Arterial Pulmonar” and “Moving toward to a omic classification for pulmonary arterial hypertension”. Instituto de Salud Carlos III, Ministerio de Economía y Competitividad, Gobierno de España. Co-funded by “Fondo Europeo de Desarrollo Regional, Programa Operativo Crecimiento Inteligente 2014–2020” (https://www.isciii.es/Paginas/Inicio.aspx). Award number: PI 18/01233, PI21-01593, and PI21-01690.
A.C.U. holds a research-training contract “Rio Hortega” (CM20/00164) from the Spanish Ministry of Science and Innovation (Instituto de Salud Carlos III).