Obtaining pleural tissue (PT) is often necessary to achieve definitive diagnosis in patients presenting with pleural effusion (PE).1 There are a variety of pleural biopsy (PB) techniques and no consensus exits regarding which needles are appropriate. The reported sensitivities vary widely depending on the population studied.2–4
Medical thoracoscopy (MT) has been shown to be a method with high diagnostic yield.5 For this reason, the use of PB for diagnosis of PE is questionable. However, image-guided PB or ultrasound-assisted PB (UAPB) can have a significantly higher accuracy, especially if there is pleural thickening (>1cm) or masses.6–8
But, the role of ultrasound to guide these biopsies is not well-defined. We would expect pleural metastases to be more frequent inferiorly in the thorax and ultrasound may be able to help identify a more suitable, lower for sampling.3 A trial in suspected tuberculous compared diagnostic yield between UAPB Abrams and Tru-cut.9 Ultrasound was used to identify the optimal sampling site and biopsies were performed without direct guidance. Diagnostic yield was higher using Abrams (91% vs 79%, p=0.015), but the data may be limited by the focus on suspected tuberculous rather than undiagnosed PE.9 Our group performed a prospective study to compare the diagnostic yield PB (no real-time biopsy) using an Abrams needle and choosing the point of entry with ultrasound. The sensitivity of UAPB in malignant PE (MPE) was 77% compared to 60% with blind PB.3
The aim of this study is to evaluate the diagnostic accuracy and safety of UAPB in a group representative of patients with PE of everyday clinical practice.
This was a observational study. The cohort comprises all patients who underwent UAPB for PE at our institution over last 3-years. Ultrasound was performed to select the site of biopsy (no real-time biopsy). The aetiology of PE was determined based on accepted criteria by guidelines.1 All patients were followed up for at least 6 months.
All procedures were performed by 2 interventional pulmonologist. The type of needle was decided by the operator. The choice of needle was not randomized and depended of characteristics radiological and needle available.
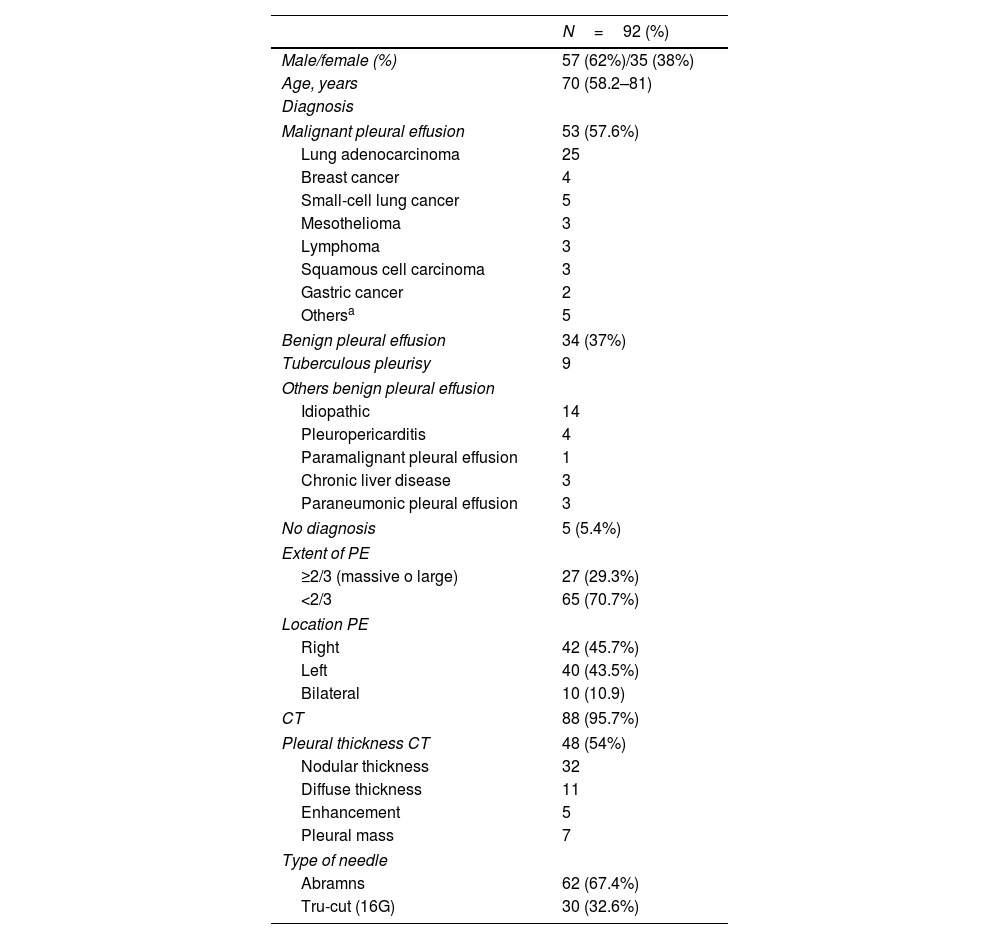
92 patients were to undergo PB (Table 1). PT was obtained in 82% [Abrams 98.4% vs Tru-cut 72%; p=0.001].
Study Population.
| N=92 (%) | |
|---|---|
| Male/female (%) | 57 (62%)/35 (38%) |
| Age, years | 70 (58.2–81) |
| Diagnosis | |
| Malignant pleural effusion | 53 (57.6%) |
| Lung adenocarcinoma | 25 |
| Breast cancer | 4 |
| Small-cell lung cancer | 5 |
| Mesothelioma | 3 |
| Lymphoma | 3 |
| Squamous cell carcinoma | 3 |
| Gastric cancer | 2 |
| Othersa | 5 |
| Benign pleural effusion | 34 (37%) |
| Tuberculous pleurisy | 9 |
| Others benign pleural effusion | |
| Idiopathic | 14 |
| Pleuropericarditis | 4 |
| Paramalignant pleural effusion | 1 |
| Chronic liver disease | 3 |
| Paraneumonic pleural effusion | 3 |
| No diagnosis | 5 (5.4%) |
| Extent of PE | |
| ≥2/3 (massive o large) | 27 (29.3%) |
| <2/3 | 65 (70.7%) |
| Location PE | |
| Right | 42 (45.7%) |
| Left | 40 (43.5%) |
| Bilateral | 10 (10.9) |
| CT | 88 (95.7%) |
| Pleural thickness CT | 48 (54%) |
| Nodular thickness | 32 |
| Diffuse thickness | 11 |
| Enhancement | 5 |
| Pleural mass | 7 |
| Type of needle | |
| Abramns | 62 (67.4%) |
| Tru-cut (16G) | 30 (32.6%) |
Abbreviations: PE=pleural effusion.
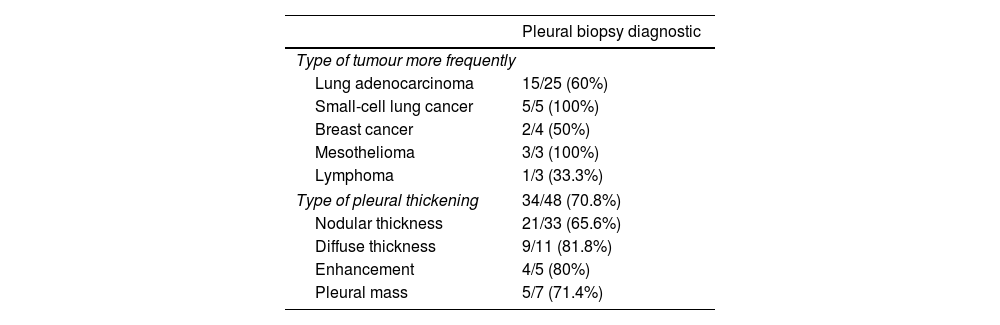
The overall accuracy of UAPB was 74% [Abrams 79% vs Tru-cut 63%; p=0.08]. The diagnostic yield in MPE was 67% [Abrams 70.6% vs Tru-cut 68.4%; p=0.5]. The biopsy contribute to the immunohistochemistry and molecular diagnosis of malignancy in all cases. In Table 2 shows the yield diagnostic for each type of tumour or pleural thickening. We perform a univariate and multivariate analysis to analyze what factors could influence in these results. The variables related to patient, radiological characteristics, type of needle and others biopsy-associated factors don’t relate with overall diagnostic yield.
Yield Diagnostic for Each Type of Tumour and Each Type of Pleural Thickening.
| Pleural biopsy diagnostic | |
|---|---|
| Type of tumour more frequently | |
| Lung adenocarcinoma | 15/25 (60%) |
| Small-cell lung cancer | 5/5 (100%) |
| Breast cancer | 2/4 (50%) |
| Mesothelioma | 3/3 (100%) |
| Lymphoma | 1/3 (33.3%) |
| Type of pleural thickening | 34/48 (70.8%) |
| Nodular thickness | 21/33 (65.6%) |
| Diffuse thickness | 9/11 (81.8%) |
| Enhancement | 4/5 (80%) |
| Pleural mass | 5/7 (71.4%) |
The diagnostic yield for tuberculous PE was 78% [Abrams 71% vs Tru-cut 100%; p=0.5]. In the group of patients with other benign PE, adequate PT were obtained in 92%. In theses two groups of patients the most of the PB were made with the Abramns needle (>75%).
Complications were in 9.8% [Abrams 11.3% vs Tru-cut 6.7%; p=0.3]. They were: Abrams: 5 cases reaction vasovagal, 1 pneumothorax that required a chest drain and 1 haemothorax required surgery; Tru-cut: 2 cases reaction vasovagal.
This is the first study to evaluate in a real setting and with unselected consecutive patients with different etiologies of PE the accuracy and safety of UAPB and to analyze potential factors the influence of yield diagnostic.
PB can be performed in a different ways2,10–12 and ultrasound is increasingly considered an essential tool for the pulmonologist.13
In our study, the yield UAPB was 74%. Ultrasound assistance in selection of site, it improved the acquisition of adequate specimens, compared to site selection via digital percussion and auscultation, independently of the existence of masses or pleural thickening.3 Pleural malignant deposits tend to predominate to the middle and diaphragm. UAPB allows biopsies to be performed in the lower thoracic parietal pleura, where the spread pleural metastasis is more likely, and may lead to improved diagnostic yield. UAPB increased by >17% in MPE.3 These results could be important for the training of new interventional pulmonologists in specific units.14
In other study, described a similar diagnostic yield for UAPB with Tru-cut (free-hand technique).15 127 UAPB were reviewed. Although it wasn’t the only main objective of the study, the yield diagnostic of UAPB was 54% for MPE.15
Koegelenberg et al.9 compared UAPB Abrams and Tru-cut needle but only for pleural tuberculous. UAPB performed with Abramns needle are more likely to contain PT and have a higher diagnostic sensitivity.9 No pneumothoraces or major haemorrhages were documented.
Zhang T et al.2 investigated the diagnostic yield of PB with a different needle in two centres of China. In this study, the sensitivity for MPE was 51% and for tuberculous 68%. But in this study, they didn’t image-guided because it can requires a higher level of training. Unlike our study, the authors excluded non-specific diagnoses, which might be malignancy or tuberculous, because we did not follow up with these patients to make a firm diagnosis.
MT is established largely and effective diagnostic procedure of PE.5 However, MT requires a degree of expertise and is not available in many hospitals, therefore, transthoracic PB can be the prefer initial procedure.3,16 Recent studies have proposed that image-guidance significantly increases the yield of such biopsies and also decreases the risk of complications.12,16–18
A randomized trial compared of the accuracy of ultrasound-guided cutting needle biopsy with a MT for tuberculous pleuritis.10 The sensitivity was, 82% and 90% (p>0.5).10 Ultrasound-guided needle biopsies seem to be safe and beneficial in patients in whom MT is not feasible.11
Few previous reports have explored factors affecting diagnostic yield of PB in large simples. Zhang et al. investigated the diagnostic accuracy of PB and analyzed the differences of influencing factors in the results.19 The pleural thickness and needle size were independently predicted diagnostic accuracy. Our study has limitations as the study of Zhang. We did not measure pleural thickening and both were retrospective studies. The selection of needles or the selection of puncture angles was not random.
PB is not free of risks, although the percentage of complications is very low, 0–10%.6,13,20 The most frequently described complications are small hematomas at the biopsy site, pneumothorax and haemothorax, both very rare complications. In our study, there were no major complications with Tru-cut needle. The risk of complications is lower than with Abramns needle.
This current study has some limitations. First, this study was conduced with a retrospective design at a single institution and this isn’t a randomized trial. Although a potential selection bias may have affected the study results, data from all subjects were consecutively collected. This research can serve to initiate prospective randomized studies.
However, this is a real-world study. To the best our knowledge, it is the first study to analyze the diagnostic yield and safety of UAPB in an unselected population of PE with different etiologies in Caucasian population.
Our results suggest that the UAPB performed by interventional pulmonologist continues to be an effective technique with a high yield diagnostic of PE. However, the Abrams needle was associated with risk of complications of greater severity and clinical relevance. The UAPB should be included in the diagnostic algorithms of PE and it could provide an alternative technique in clinical practice, especially for hospital without MT.
Conflict of InterestNone.