Bronchiectasis is a complex and heterogeneous disorder and one of the most frequent chronic inflammatory airway diseases.1–4 It is defined as a chronic airway disorder characterized by a dilation of the airway lumen as a consequence of the inflammation (predominantly neutrophilic5,6 but also eosinophil and lymphocytic7,8) and, in many patients, chronic infection by pathogenic microorganism (mainly bacteria)9–11 with secondary symptoms mostly comprise chronic productive cough and multiple exacerbations.12,13 Until two decades ago, there were no patient registries or guidelines on it, so our knowledge of this disease, and more particularly its natural history, was extremely limited. At the beginning of the 20th century (2002) the first registry of bronchiectasis was launched in Spain,14 and in 2008 the first guidelines were also published, again in Spain.15 Although many aspects of bronchiectasis are still unknown, significant progress has been made over the last 20 years. In Spain, we have complete data on more than 4700 patients with bronchiectasis, collected in two periods spanning two decades, allowing us to analyze changes in the characteristics of patients with bronchiectasis during this long period.14,16 Therefore, the main objective of this study is to assess the changes produced in various aspects of patients with bronchiectasis over the last 20 years.
Data from the two bronchiectasis registries available in Spain were compared with respect to general characteristics (age, gender, body mass index [BMI] and smoking status) and the following aspects: diagnostic (diagnostic delay); aetiological (most frequent etiologies, including asthma and chronic obstructive pulmonary disease [COPD]); clinical (cough, dyspnea according to mMRC scale, expectoration and number of exacerbations and hospitalization in the year prior to inclusion in the registry); functional (FEV1 and FVC, %pred); microbiological (presence of chronic bronchial infection by the most frequent pathogenic microorganisms and percentage of non-tuberculous mycobacteria [NTM] isolation); severity (measured by the three validated multidimensional grading systems: FACED,17 E-FACED18 and bronchiectasis severity index [BSI])19; and therapeutic (use of inhaled corticosteroids [ICs], bronchodilators and inhaled antibiotics). The first was the historical registry of bronchiectasis and covered data obtained from 2002 to 2011 from 2099 patients from 36 hospitals.14 The second is the current Spanish computerized registry of bronchiectasis (RIBRON), containing data collected between 2015 and 2023 from 2615 patients from 43 hospitals.16,20 All the data were prospectively entered and the diagnosis of bronchiectasis was established as the primary diagnosis by high-resolution computed tomography (HRCT) in all cases. Variables were expressed as mean (standard deviation) or percentages, and the data from both registries were compared using the chi square, t-student or U-Mann Whitney tests, depending on the distribution of the variables.
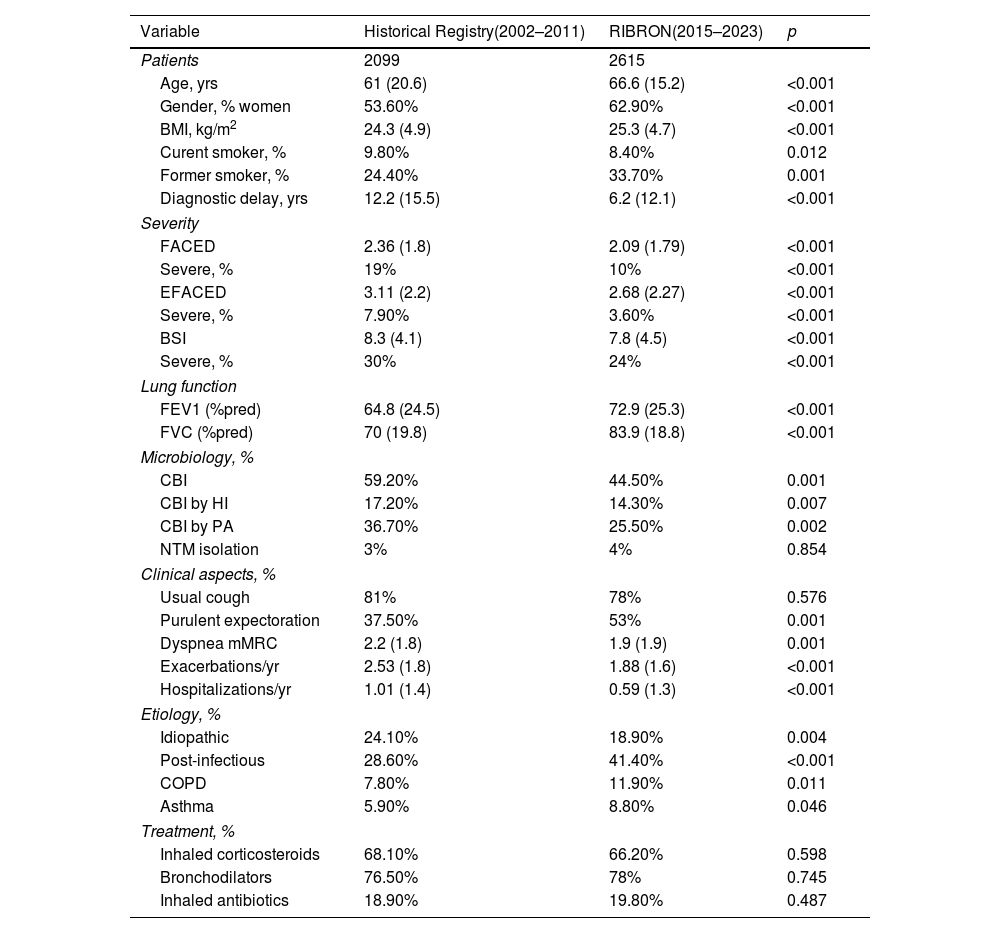
Table 1 shows the main results after comparing the characteristics of the patients between both periods. In general, there was a significant trend in all disease domains toward a decrease in disease severity over time. Thus, it can be seen that, compared to the old registry, the patients in the current registry are significantly older and present a higher proportion of women, a higher BMI, a higher percentage of etiologies that are post-infectious or related to COPD and asthma, but a lower percentage of idiopathic etiologies, less clinical severity, better pulmonary function and less severity (according to the three validated multidimensional scores). Likewise, it was observed that the percentage of chronic bronchial infection (CBI) by potentially pathogenic microorganisms, and in particular by Haemophilus influenzae and Pseudomonas aeruginosa, decreased significantly, although up to a quarter of the current patients with bronchiectasis still present CBI by P. aeruginosa. However, NTM detection remained low throughout this period of time. Possibly the most striking findings were significant decreases in the number and severity of exacerbations and in the number of years needed until diagnosis from the onset of symptoms, which went from 12.2 years in the period between 2002 and 2012 to 6.2 years in the period from 2015 to 2023 (almost half the time). Finally, it should be noted that no significant changes were observed in the percentage of patients in whom ICs, bronchodilators and inhaled antibiotics were used.
Comparison Between the Characteristics of the Patients When Comparing the Historical Record (2002–2011) and the Current Record (2015–2023).
| Variable | Historical Registry(2002–2011) | RIBRON(2015–2023) | p |
|---|---|---|---|
| Patients | 2099 | 2615 | |
| Age, yrs | 61 (20.6) | 66.6 (15.2) | <0.001 |
| Gender, % women | 53.60% | 62.90% | <0.001 |
| BMI, kg/m2 | 24.3 (4.9) | 25.3 (4.7) | <0.001 |
| Curent smoker, % | 9.80% | 8.40% | 0.012 |
| Former smoker, % | 24.40% | 33.70% | 0.001 |
| Diagnostic delay, yrs | 12.2 (15.5) | 6.2 (12.1) | <0.001 |
| Severity | |||
| FACED | 2.36 (1.8) | 2.09 (1.79) | <0.001 |
| Severe, % | 19% | 10% | <0.001 |
| EFACED | 3.11 (2.2) | 2.68 (2.27) | <0.001 |
| Severe, % | 7.90% | 3.60% | <0.001 |
| BSI | 8.3 (4.1) | 7.8 (4.5) | <0.001 |
| Severe, % | 30% | 24% | <0.001 |
| Lung function | |||
| FEV1 (%pred) | 64.8 (24.5) | 72.9 (25.3) | <0.001 |
| FVC (%pred) | 70 (19.8) | 83.9 (18.8) | <0.001 |
| Microbiology, % | |||
| CBI | 59.20% | 44.50% | 0.001 |
| CBI by HI | 17.20% | 14.30% | 0.007 |
| CBI by PA | 36.70% | 25.50% | 0.002 |
| NTM isolation | 3% | 4% | 0.854 |
| Clinical aspects, % | |||
| Usual cough | 81% | 78% | 0.576 |
| Purulent expectoration | 37.50% | 53% | 0.001 |
| Dyspnea mMRC | 2.2 (1.8) | 1.9 (1.9) | 0.001 |
| Exacerbations/yr | 2.53 (1.8) | 1.88 (1.6) | <0.001 |
| Hospitalizations/yr | 1.01 (1.4) | 0.59 (1.3) | <0.001 |
| Etiology, % | |||
| Idiopathic | 24.10% | 18.90% | 0.004 |
| Post-infectious | 28.60% | 41.40% | <0.001 |
| COPD | 7.80% | 11.90% | 0.011 |
| Asthma | 5.90% | 8.80% | 0.046 |
| Treatment, % | |||
| Inhaled corticosteroids | 68.10% | 66.20% | 0.598 |
| Bronchodilators | 76.50% | 78% | 0.745 |
| Inhaled antibiotics | 18.90% | 19.80% | 0.487 |
Data is presented as mean (standard deviation) or percentage.
BMI: body mass index; BSI: bronchiectasis severity index; CBI: chronic bronchial infection; NTM: non-tuberculous mycobacteria; HI: Haemophilus influenzae; PA: Pseudomonas aeruginosa; mMRC: modified Medical Research Council; COPD: chronic obstructive pulmonary disease; FVC: forced volume capacity.
Our results show that in the last two decades there has been a significant decrease in the general severity of bronchiectasis (fundamentally measured by multidimensional scores), as well as in the clinical aspects and the number and severity of exacerbations, despite the fact that the mean age on inclusion in the registry has increased significantly. This decrease in bronchiectasis severity is probably due to the fact that bronchiectasis is now detected earlier (the average number of years from the onset of symptoms to diagnosis was halved), leading to early diagnosis and, consequently, early treatment, with a subsequent decrease in CBI by pathogenic microorganisms.14 This early detection may be the result of greater awareness in the health community of the importance of bronchiectasis, thanks to the appearance of guidelines and registries all over the world in recent years.1,21–25
Another striking feature is the change in the etiological profile of bronchiectasis over time, with an increase in the percentage of overlap with COPD and asthma, probably as a result of the greater number of studies on those overlap syndromes produced in recent years.26 Moreover, an increase in post-infectious etiology and a decrease in idiopathic etiology have also been observed. This finding could be explained by the major etiological study that has been routinely carried out in Spanish hospitals on patients with bronchiectasis since the advent of guidelines and the proposed etiological algorithm. However, it cannot be ruled out that some cases of idiopathic bronchiectasis have been considered post-infectious infections, since their percentage also rose significantly in the second period, compared to the first.
Finally, it is important to highlight that the use of ICs is excessively high in patients with bronchiectasis and has not changed over time13,15,27; this cannot be explained by the increase in the number of overlapping patients with COPD and asthma. Although the possible role of the peripheral eosinophil count in patients with bronchiectasis has been studied with respect to the response to ICs in recent years,28 it is evident that the excessive use of these drugs in bronchiectasis needs to be reconsidered, since it is not devoid of adverse effects.
The greatest strength of this study is its insight into the changes produced in the characteristics of bronchiectasis over approximately two decades in a large series of patients. Among the limitations, it should be noted that the data come entirely from Spain, so they may not be extrapolated to other countries where the experience, forms of presentation, etiological spectrum and management may be different.
In summary, in the last 20 years, the severity of bronchiectasis in Spain has probably decreased as a consequence of significantly earlier detection of the disease, which allows for early treatment. The role of ICs remains a problem that must be solved, due to their excessive use.
Conflict of InterestsThe author states that they have no conflict of interests.