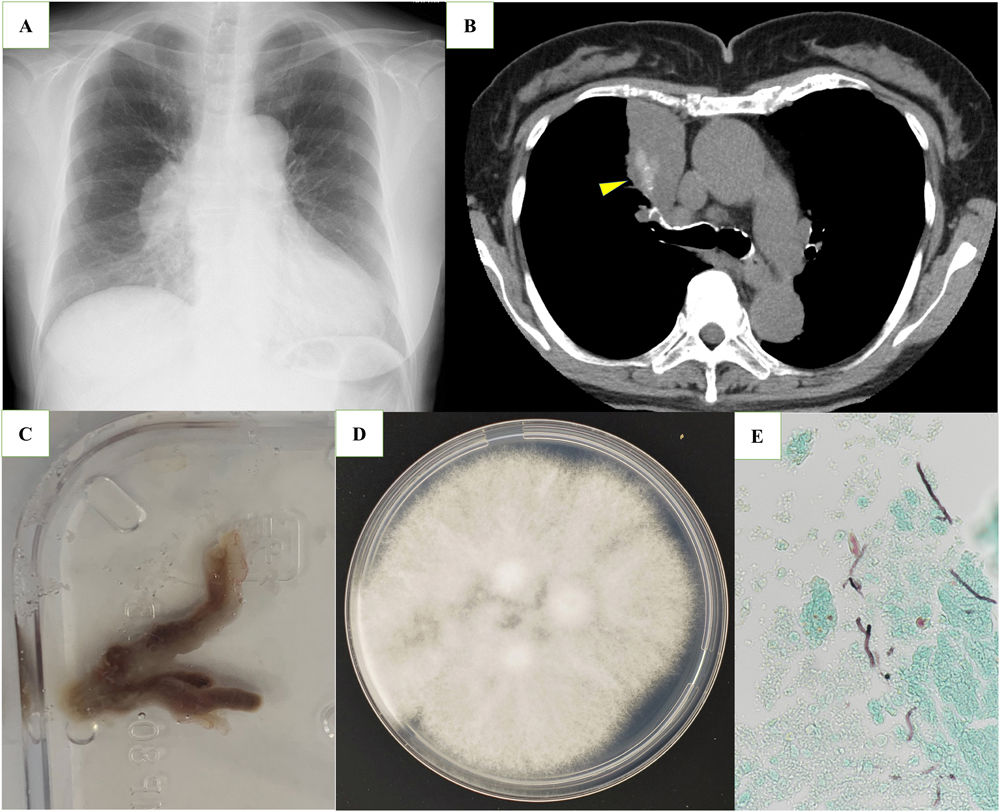
A 73-year-old woman presented with right precordial pleuritic pain. Chest X-ray showed a lung mass shadow on the right lower hilum (Fig. 1a). Neoplastic lesions were suspected. Chest computed tomography revealed bronchial cast shadows with high-attenuation lesions in the right upper lobe (Fig. 1b) and central bronchiectasis. A purulent mucous plug was aspirated from the origin of the right upper bronchus (Fig. 1c). Culture of the aspirated mucus showed growth of a fungus (Fig. 1d), which was identified as Schizophyllum commune by polymerase chain reaction amplification of the internal transcribed spacer region of the ribosomal DNA. She had no history of bronchial asthma and lung function test did not show the airflow limitation. Peripheral blood eosinophilia was detected (873/mL). Specific immunoglobulin G antibody to S. commune was positive. Total immunoglobulin E was normal (27.3IU/mL) and serum specific IgE antibody was negative (1.98UA/ml). Histopathological examination showed fungal hyphae (Fig. 1e). Although this case had no manifestation of asthma, ABPM associated with S. commune was diagnosed based on the new diagnostic criteria recently proposed in Japan.1 Recently, numerous fungi other than Aspergillus spp. have been implicated in the etiology of ABPM.2
(a) Chest X ray shows tumor-like shadow in the right lower hilum. (b) Chest computed tomography shows high attenuation in the right upper lobe (yellow arrow head). (c) Purulent mucus plug aspirated by bronchoscopy. (d) Woolly, whitish to pale greyish-brown colony of Schizophyllum commune on potato dextrose agar after 7 days of incubation at 25°C. (e) Grocott Gomori Methanamine Silver staining of mucus plug showing fungal hyphae (×400).
ABPM should be considered as a different diagnosis of lung mass lesions on chest X-ray.
We thank Takashi Yaguchi (Medical Mycology Research Center, Chiba University) for his contribution to identification of causative fungus through the National Bio-Resource Project, Japan, and Hiroshi Shimazu (Department of Hematology, Mishuku Hospital) for his contribution to patient treatment.