Continuous positive airway pressure (CPAP) therapy is the gold standard treatment for obstructive sleep apnea (OSA). Favorable outcomes, such as decreased blood pressure, reduced stroke risk, and decreased daytime sleepiness, depend on adherence to CPAP therapy.1,2 However, rates of non-adherence to CPAP therapy range from 30% to 40%.3 Factors that influence adherence to CPAP therapy include disease and patient characteristics, psychological and social factors, and side effects.4 Additionally, temperature, which is a seasonal factor, also influences adherence to CPAP therapy.5 Cold, arid air, especially in winter, affects the adherence to CPAP caused by issues, such as nasal congestion, dryness of the nose and throat, and sneezing.6,7 To address this and to mitigate cold air and dryness delivered by CPAP devices, a heated humidifier and breathing tube have been developed. However, literature regarding the impact of high temperatures on CPAP therapy adherence is limited globally. Fujino et al. reported that the CPAP usage rate for ≥4h daily and the duration of daily CPAP use were worst in summer among patients with OSA receiving CPAP therapy in Japan.5 They concluded that a high temperature could decrease the adherence rate to CPAP therapy. However, no machines for cooling hot air from CPAP devices have been developed. This present study was an experimental trial to evaluate whether a cooling towel could serve as a novel cooling system in CPAP therapy.
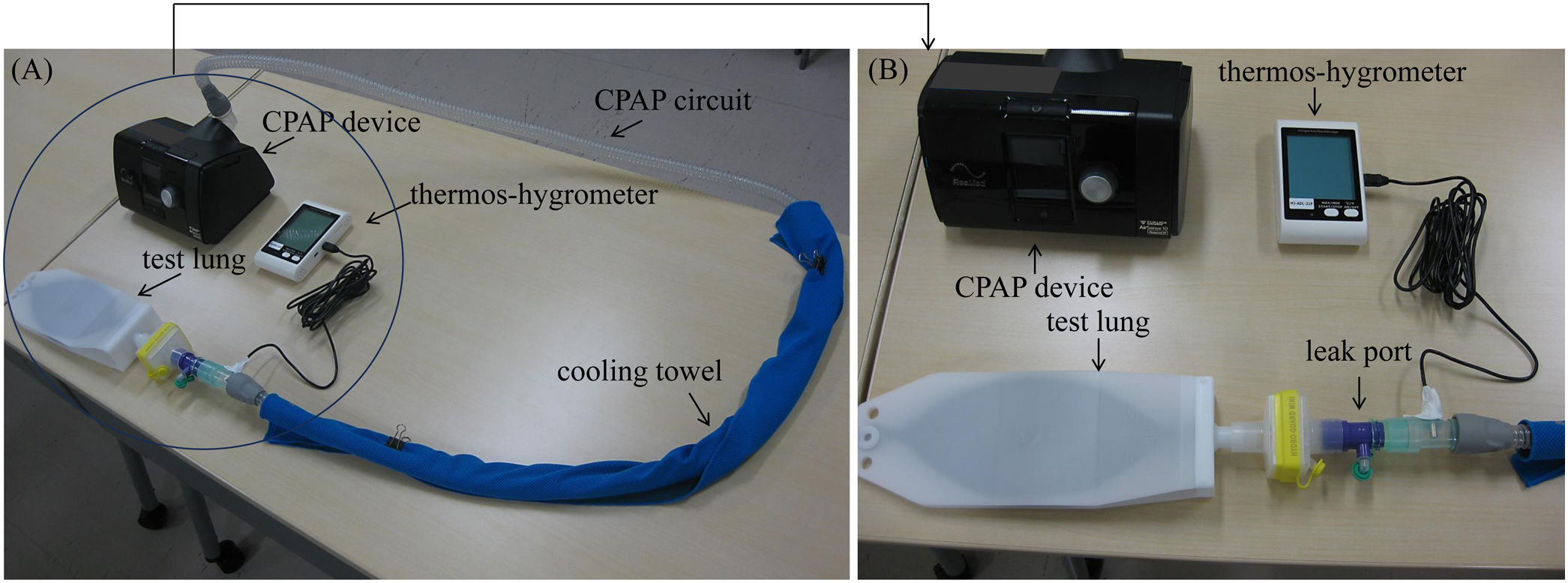
First, we preformed a bench study to examine the change in temperature and humidity within the circuit of a CPAP device (AirSence10 Respond; ResMed®, Sydney, Australia) using a thermos-hygrometer (MJ-ADL-21P, SATO SHOUJI INC, Kanagawa, Japan), which enabled continuous monitoring of temperature and relative humidity every 10s (Fig. 1). A cooling towel (COOLCORE®: ITOCHU Corporation, Tokyo, Japan), which was wetted and squeezed, was wrapped around the circuit of the CPAP device (Fig. 1). The CPAP device was set to a fixed pressure of 10cmH2O and placed in an incubator (size: 80cm [width]×40cm [depth]×45cm [height]), within which the temperature was set at 26, 28, or 30°C.
Second, we provided a cooling towel to five patients with OSA (four using CPAP device and 1 using servo-ventilation [SV] device) from July to September who complained of the hot air from the CPAP and SV devices. All patients did not use a heated humidifier or heated breathing tube and did not use an air conditioner at night. Patients were asked about changes in their perceptions of air supplied via the CPAP and SV devices at an outpatient clinic from 1 to 3 months after providing the cooling towel, and changes in temperature and humidity were categorized as follows: 1, freezing and dry; 2, somewhat cold and dry; 3, no change; 4, somewhat hot and wet; and 5, very hot and wet. Written informed consent was obtained from all patients.
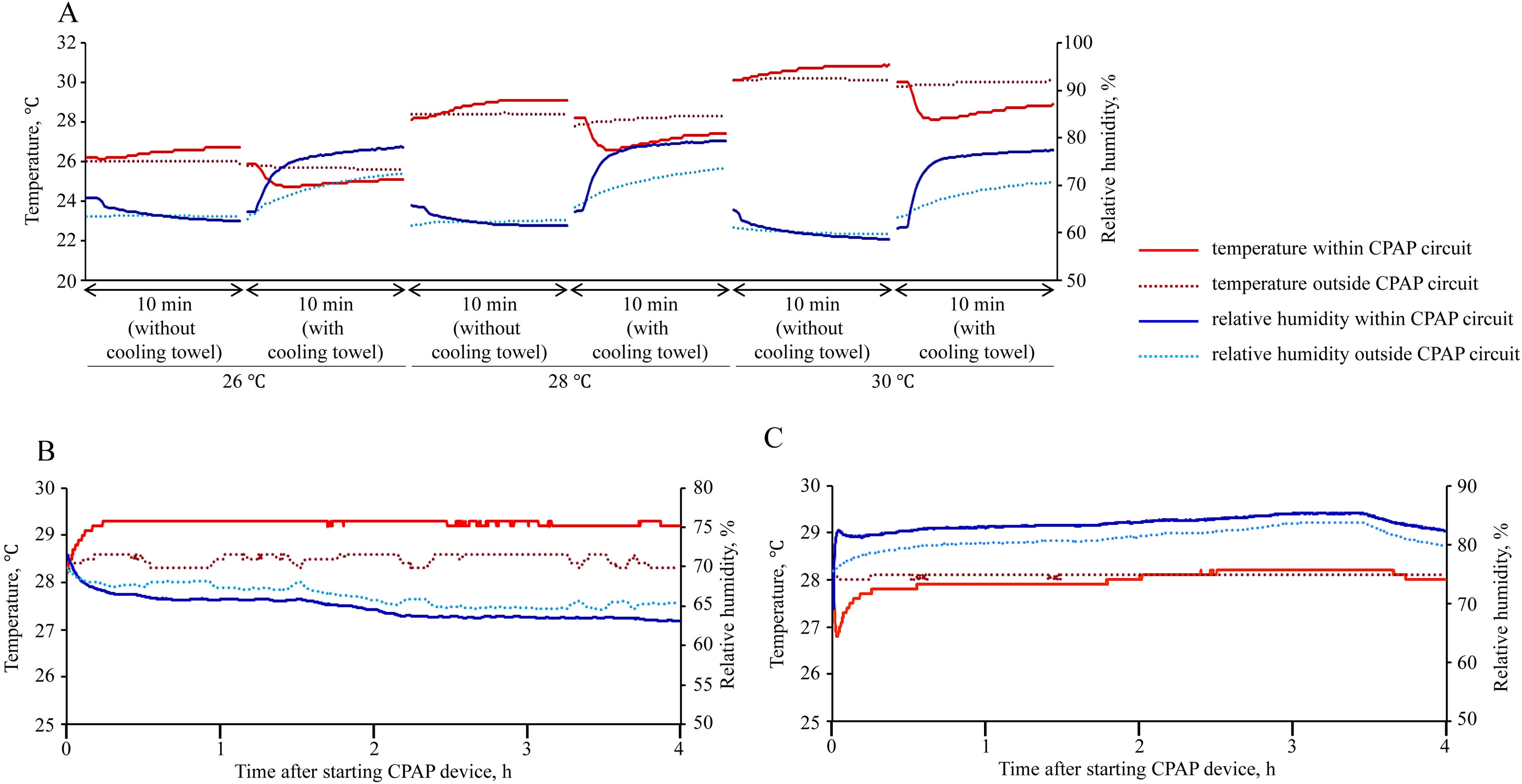
Fig. 2A shows the change in temperature and relative humidity within and outside the CPAP circuit. The experimental settings, including temperature within the incubator (26, 28, or 30°C) and attachment of the cooling towel, were changed every 10min. In the absence of the cooling towel, temperature within the CPAP circuit gradually rose (from 26.2 to 26.7°C at 26°C, from 28.1 to 29.1°C at 28°C, and from 30.1 to 30.9°C at 30°C), compared to external temperature an increase of 0.8°C, 0.7°C, and 0.8°C was observed at temperatures of 26°C, 28°C, and 30°C, respectively. When using the cooling towel, temperature within the CPAP circuit swiftly decreased (from 25.9 to 24.9°C at 26°C, from 28.2 to 26.9°C at 28°C, and from 30.0 to 28.5°C at 30°C), compared to external temperature, reductions of 0.5°C, 0.9°C, and 1.2°C was observed at temperatures of 26°C, 28°C, and 30°C, respectively. In terms of relative humidity, without the cooling towel, levels within the CPAP circuit gradually decreased from 67.3 to 62.4% (26°C), from 65.7 to 61.6% (28°C), and from 64.8 to 58.6 (30°C), resulting in decreases of 1% (26°C), 1.1% (28°C), and 1% (30°C) compared to external levels. However, with the cooling towel, relative humidity within the CPAP circuit rapidly increased from 64.4 to 78.0% (26°C), from 64.5 to 79.4% (28°C), and from 61.0 to 77.5% (30°C), resulting in increases of 5.5% (26°C), 5.8% (28°C), and 6.8% (30°C) compared to external levels.
Fig. 2B (without the cooling towel) and C (with the cooling towel) shows the changes in temperature and relative humidity within and outside the CPAP circuit at a temperature of 28°C within the incubator for 4h. In the absence of the cooling towel, the temperature within the CPAP circuit showed a gradual increase from 28.3°C to 29.3°C within 15min of activating the CPAP device, ultimately increasing the temperature by 0.9°C in comparison to the external temperature. Concurrently, the relative humidity decreased from 71.5% to 63.1%, ultimately reducing the humidity by 2.3% compared to external levels. Conversely, with the cooling towel, the temperature initially decreased within 6min of starting the CPAP device, then stabilized at 28°C. Simultaneously, the relative humidity within the CPAP circuit showed a rapid increase from 69.4 to 82.4% within 6min of starting the CPAP device, followed by a steady increase, ultimately increasing by 2.5% compared to external levels.
Among the five patients, two felt somewhat cold air, whereas the other three did not report any changes in the air temperature; however, one felt somewhat cold air immediately after switching CPAP device on. Regarding humidity, all patients did not feel any changes. Meanwhile, two patients experienced moisture of the cooling towel, which resulted in bedwetting.
This study revealed three novel findings. First, after initiating the CPAP device, the temperature increased within the CPAP circuit, while the relative humidity within steadily decreased. Second, under wrapping the CPAP circuit with the cooling towel, the temperature within the CPAP circuit rapidly decreased and increased thereafter but not above the set temperature, while the relative humidity increased. The effect of the cooling towel on temperature and humidity is considered secondary to evaporation. Third, in the five patients on CPAP therapy, two felt somewhat cold of air from the CPAP devices. The cooling towel costs approximately 1000 Yen (6.2 Euro). Thus, the cooling towel could become a novel and cost-effective cooling system for CPAP device. However, the impact of the cooling towel on pressure variations in CPAP devices, management of OSA, and adherence to CPAP therapy has been investigated. Consequently, future clinical research incorporating the use of the cooling towel in clinical settings is warranted.
While there are regional and ethical differences regarding the use air conditioners at night, Japanese tend to not use them, which could influence adherence to CPAP therapy in summer in Japan.5 However, as described above, no machines for cooling hot air from CPAP devices have been developed. As global warming has progressed, techniques to cool the hot air from CPAP devices are needed. A cooling towel is a novel and cost-effective method to cool hot air from CPAP devices; however, it causes moisture, which results in bedwetting, and lowers the temperature of the CPAP circuit, albeit temporarily. Thus, technological development in cooling towel application is needed.
In conclusion, a cooling towel is a novel and cost-effective cooling system in CPAP therapy.
Financial conflictsThe Department of Advanced Medicine for Respiratory Failure is a Department of Collaborative Research Laboratory funded by Teijin Pharma.
The Department of Respiratory Care and Sleep Control Medicine is funded by endowments from Philips-Respironics, ResMed, Fukuda Denshi and Fukuda Lifetec-Keiji to Kyoto University.
This study was funded in part by the JSPS KAKENHI 22K16169 (SH).
Conflict of interestSatoshi Hamada reports grants from Teijin Pharma, outside the submitted work.
Susumu Sato reports grants from Philips Japan, ResMed, Fukuda Denshi, Fukuda Lifetec Keiji, Fuji Film corporation, and Nippon Boehringer Ingelheim, outside the submitted work.
Jumpei Togawa, Hironobu Sunadome, and Naomi Takahashi report grants from Philips Japan, ResMed, Fukuda Denshi, and Fukuda Lifetec Keiji, outside the submitted work.
Toyohiro Hirai has nothing to disclosure.
We have no acknowledgements.