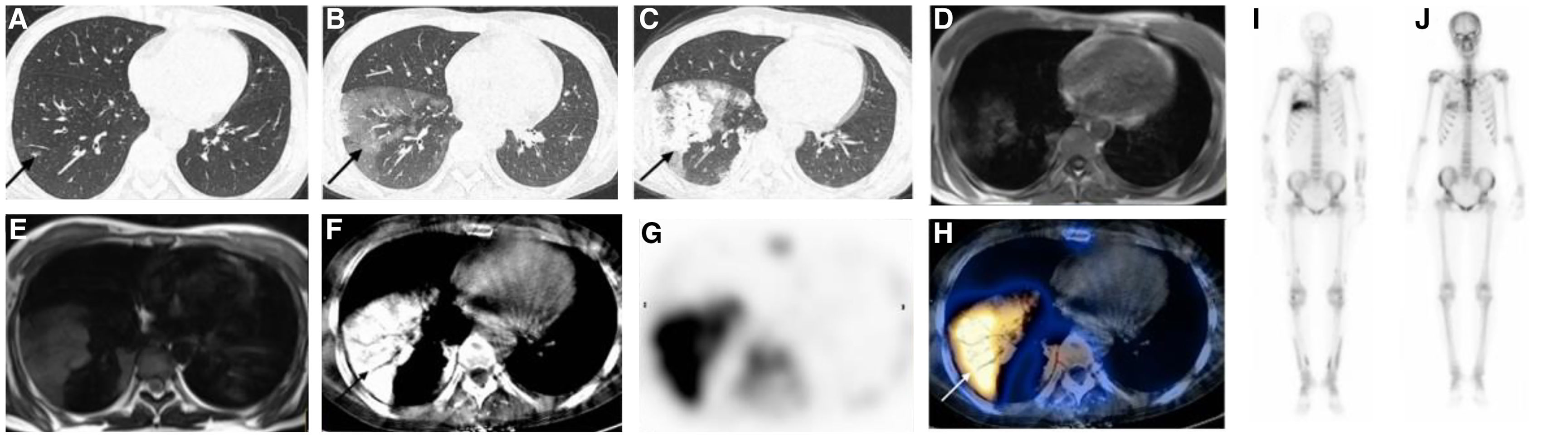
We report the case of a 24-year-old woman with chronic kidney disease and maintenance peritoneal dialysis for 4 years who was admitted to our hospital due to inadequate drainage of the peritoneal dialysis tube. There were no respiratory symptoms during the hospitalization, but coughing symptoms appeared after anti-infective therapy in the case of imaging abnormalities, but no fever. The first computed tomography (CT) of the chest showed patchy areas of ground-glass opacity in the lower leaf of the right lung (Fig. 1A). Half a month later, the lesion turned into diffuse and patchy areas of consolidation (Fig. 1B). The lesions were expanded, and the density was significantly increased after one week of anti-infective treatment (Fig. 1C). The magnetic resonance showed uneven equal T1 and equal T2 signals, indicating the deposition of paramagnetic material (Fig. 1D and E). The bone scintigraphy imaging demonstrated increased radioactive isotope uptake on the right lung and subcutaneous soft tissue layer of the extremities, suggesting metastatic calcification (Fig. 1F–I), which was also consistent with the lung puncture pathology that demonstrated calcium deposition. Metastatic pulmonary calcification was finally diagnosed based on bone scintigraphy imaging and pathology. After treatment with sodium thiosulfate and follow-up for 8 months, bone scintigraphy showed a significant decrease in radiation uptake in right lung lesions (Fig. 1J).
(A) Chest CT scan in the lung window. Patchy areas of ground-glass opacity in the lower leaf of right lung (arrow). (B) Half a month later, chest CT scan in the lung window showed diffuse and patchy areas of consolidation (arrow). (C) The density was significantly increased after anti-infective treatment for a period of time (arrows). (D and E) The magnetic resonance: showed uneven equal T1 and equal T2 signals. (F–H) SPECT/CT: the bone scintigraphy imaging demonstrated increased radioactive isotope uptake on the right lung, and subcutaneous soft tissue layer of the extremities. (J) Bone scintigraphy showed a significant decrease in radiation uptake in right lung lesions after treatment with sodium thiosulfate.
Progressive metastatic pulmonary calcification (MPC), a rare and serious complication of chronic renal failure, is the result of calcium salts deposition in the alveolar epithelial basement membranes,1 and occurs in the setting of chronic renal failure, hyperparathyroidism, metastatic neoplasms, hypervitaminosis D, and hypercalcemia of other origins.2 Patients with MPC may be asymptomatic, while others with subtle calcification may have severe respiratory compromise.3 So the early diagnosis of MPC is important. While, the early findings on chest CT may be confused with pulmonary oedema and pneumonia. The 99mTc-methylene diphosphonate (MDP) bone scintigraphy binding to calcium by chemisorption and using single photon emission computed tomography/computed tomography (SPECT/CT) with high sensitivity, might be a useful instrument in the initial evaluation and follow-up of patients with a high risk of developing metastatic calcification, even in the detection of early changes.4 And perhaps obviating the need for invasive diagnostic procedures. Sodium thiosulfate, which sequesters calcium ions to form highly soluble calcium thiosulfate complexes, can prevent calcium phosphate precipitation.5
From what has been discussed above, MPC should be considered when dialysis patients develop unexplained radiographic changes. To carry out clinical treatment earlier.
Authors’ ContributionsShan Huang and Fei Li contributed equally to this work.
FundingNone declared.
Conflicts of InterestThe authors state that they have no conflict of interests.