Paget-Schroetter syndrome (PSS) in the context of upper extremity deep venous thrombosis (DVT) is an uncommon but potentially very serious condition affecting young, healthy adults, in which secondary post-thrombotic syndrome (PTS) can be a complication with major implications. The best treatment option remains controversial, with current guidelines recommending anticoagulation for at least 3 months. However, an incidence of PTS of approximately 50% after 6 months, 30% after 1 year and 25% after 2 years has been found using this therapeutic approach. Consequently, specialized units recommend local thrombolysis and early decompressive surgery. We describe a series of eight cases treated in this way. None of the patients showed signs of complications, and an early return to regular activities with no PTS was observed in 90% of cases.
El síndrome de Paget-Schroetter (SPS) en el contexto de trombosis venosa profunda (TVP) de miembro superior es una patología poco frecuente pero de gran importancia por afectar personas sanas y jóvenes, donde el síndrome postrombótico (SPT) secundario puede ser una complicación con importantes implicaciones. La mejor opción de tratamiento es controvertida. Las guías actuales recomiendan anticoagulación durante un mínimo de 3 meses, aunque se han visto con este manejo incidencias de SPT cercanas al 50% a los 6 meses, al 30% al año y al 25% a los 2 años, por lo que unidades especializadas abogan por la realización de trombólisis local y cirugía descompresiva precoz, con el propósito de disminuir estas cifras. Describimos una serie de 8 casos, a los que tratamos de esta última manera. Ningún paciente presentó complicaciones, y en todos se observó reintegro precoz a la actividad diaria, con ausencia de SPT en el 90% de ellos.
Paget-Schroetter syndrome (PSS) refers to primary deep vein thrombosis (DVT) at the costoclavicular junction, where the subclavian vein is highly vulnerable to injury as it passes by the junction of the first rib and clavicle in the most anterior part of the thoracic outlet. Repetitive forced abduction and retroversion movements of the arm can damage the innermost layer of the vessel, generating a thrombogenic surface and extrinsic scar tissue, which triggers this entity.1
PSS has an estimated prevalence of around 30% of cases of upper extremity DVT and 1%–4% of all DVT; the mean age at presentation is between 30 and 40 years, predominantly in men, in the dominant upper limb, and in relation to activities requiring effort.2,3
Clinical manifestations vary in severity, but the disease generally presents as axillo-humeral pain, edema in the extremity, cyanosis and collateral circulation at shoulder level.
Doppler ultrasound is usually the first diagnostic test, with specificity of 93% and sensitivity greater than 80%.3,4 Other imaging studies, such as computed tomography (CT) or nuclear magnetic resonance imaging (MRI) are suitable for investigating other causes of compression or confirming the diagnosis when there is high suspicion of the condition, but normal ultrasound findings (Table 1).
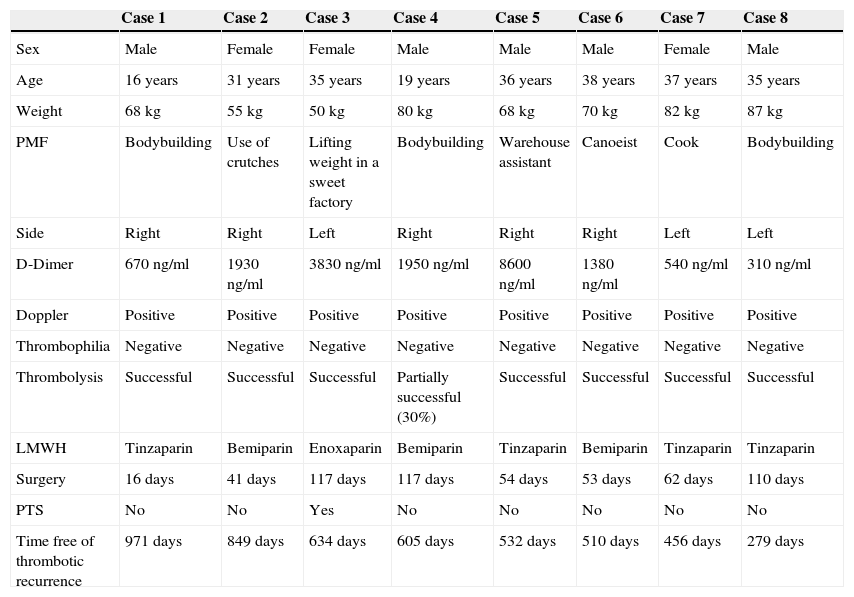
Clinical Characteristics of Patients Included in the Study.
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | |
|---|---|---|---|---|---|---|---|---|
| Sex | Male | Female | Female | Male | Male | Male | Female | Male |
| Age | 16 years | 31 years | 35 years | 19 years | 36 years | 38 years | 37 years | 35 years |
| Weight | 68kg | 55kg | 50kg | 80kg | 68kg | 70kg | 82kg | 87kg |
| PMF | Bodybuilding | Use of crutches | Lifting weight in a sweet factory | Bodybuilding | Warehouse assistant | Canoeist | Cook | Bodybuilding |
| Side | Right | Right | Left | Right | Right | Right | Left | Left |
| D-Dimer | 670ng/ml | 1930ng/ml | 3830ng/ml | 1950ng/ml | 8600ng/ml | 1380ng/ml | 540ng/ml | 310ng/ml |
| Doppler | Positive | Positive | Positive | Positive | Positive | Positive | Positive | Positive |
| Thrombophilia | Negative | Negative | Negative | Negative | Negative | Negative | Negative | Negative |
| Thrombolysis | Successful | Successful | Successful | Partially successful (30%) | Successful | Successful | Successful | Successful |
| LMWH | Tinzaparin | Bemiparin | Enoxaparin | Bemiparin | Tinzaparin | Bemiparin | Tinzaparin | Tinzaparin |
| Surgery | 16 days | 41 days | 117 days | 117 days | 54 days | 53 days | 62 days | 110 days |
| PTS | No | No | Yes | No | No | No | No | No |
| Time free of thrombotic recurrence | 971 days | 849 days | 634 days | 605 days | 532 days | 510 days | 456 days | 279 days |
PMF: predisposing mechanical factor.
When not treated promptly, an intraluminal fibrotic reaction is generated that leads to chronic venous hypertension and onset of post-thrombotic syndrome (PTS), which in some cases can cause significant functional discapacity and severely impair quality of life.3
The most effective therapeutic strategy is controversial. Current guidelines recommend conventional anticoagulation, although they consider the possibility of catheter-guided local thrombolysis and thoracic outlet release surgery in experienced centers.5
Clinical ObservationA prospective study was conducted between November 2011 and May 2013 in 5 men and 3 women with acute symptoms consistent with PSS, in whom DVT was confirmed by Doppler ultrasound. After admission, an established protocol was applied, which included:
- -
Detailed medical history.
- -
Complete laboratory workup with D-dimer.
- -
Dynamic CT of the affected limb.
- -
Initial venography with placement of a multihole catheter upstream of the occlusion, using the basilic vein approach.
- -
Local thrombolysis with urokinase (100000IU/100ml/h).
- -
Follow-up venography. The thrombolysis is considered successful if no residual thrombus is detected on the follow-up venography, partially successful if the persistent thrombus is less than 50% of the initial thrombus, and unsuccessful if the persistent thrombus is greater than 50% of the initial thrombus.
- -
Low molecular weight heparin (LMWH) at therapeutic doses.
- -
Thoracic outlet decompression surgery, which included disinsertion of the anterior scalene muscle and transaxillary first rib resection, as per the Roos technique, within 16 weeks of diagnosis.
- -
LMWH for 1 month at therapeutic doses.
- -
Thrombophilia study 3 months after the surgery.
- -
Clinical follow-up every 6 months to date, with assessment of the PTS using the Villalta scale6 at each follow-up visit.
Following implementation of the protocol, none of the patients have presented complications or thrombotic recurrences to date. One of the 8 patients presented mild PTS on the Villalta scale, although this did not prevent him from carrying out his daily work activities.
DiscussionFor many years, the treatment of PSS has included elevation of the extremity and anticoagulation, with surgery considered only when symptoms recur.1,4 Current guidelines recommend initial treatment with parenteral anticoagulation for at least 3 months, over no such initial treatment. Similarly, in selected patients with a low risk for bleeding and severe symptoms of recent onset, catheter-directed thrombolysis is recommended in experienced centers. First rib resection and scalene muscle disinsertion when subclavian vein entrapment is suspected are also recommended.5
The use of anticoagulants as monotherapy is now being questioned after some studies found residual venous obstruction in close to 80% of patients, and persistent venous congestion symptoms in up to 90% of patients receiving this treatment.4
Opinions differ with regard to the best time to perform surgery. However, studies with longer series have compared surgical times and found that thrombolysis followed by early surgery is the strategy with the best clinical outcomes.5,7
ConclusionsPSS is a rare entity affecting young, healthy individuals, and early diagnosis is the key to obtaining adequate venous patency. In our case series, early diagnosis and treatment, following the recommendations of the most advanced studies, has so far led to favorable evolution and outcomes in our patients. Multidisciplinary management using local catheter-directed thrombolysis and early decompressive surgery performed by an experienced multidisciplinary medical team shows satisfactory results, with no major complications and a far lower incidence of PTS compared with conservative treatment.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Rosa Salazar V, Otálora Valderrama SP, Hernández Contreras ME, García Pérez B, Arroyo Tristán AA, García Méndez MM. Manejo multidisciplinar del síndrome de Paget-Schroetter. A propósito de una serie de 8 casos. Arch Bronconeumol. 2015;51:e41–e43.