In 2008, a 78-year-old man was referred to us for observation, after detecting a mediastinal mass with size progression located in the right hemithorax. The patient reported a 2-year history of mild dysphagia, associated with exertional dyspnea for the previous 6 months. His medical history included hypertension and inguinal hernia repair ten years earlier.
The physical examination was unremarkable; neck palpation in particular did not reveal cervical masses and the tracheal axis occupied the midline of the neck. Laboratory test results were normal, except for the serum calcium concentration, which was 14.2mg/dl (normal 8.0–10.5mg/dl) and phosphorus concentration, which was 1.9mg/dl (normal 2.5–4.45mg/dl). The serum parathormone (PTH) concentration was six times higher than the upper limit of normal. The spirometry was indicative of possible upper airway obstruction.
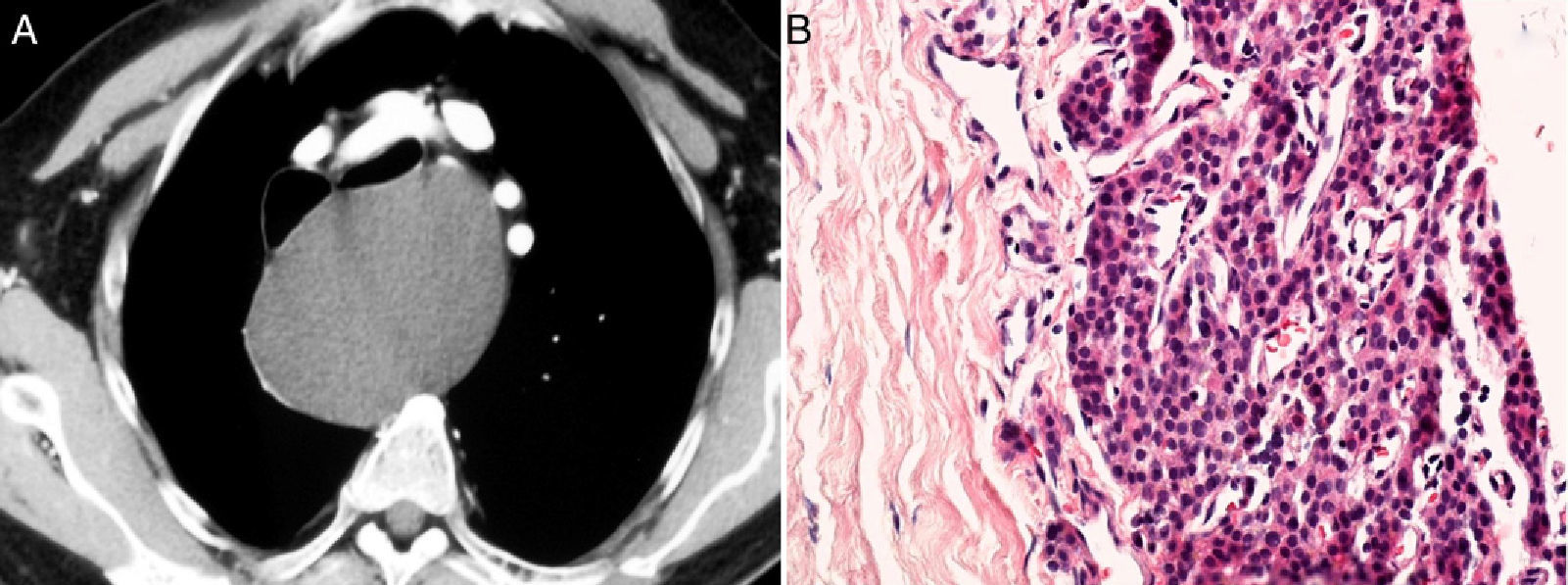
The chest radiograph showed the presence of a right mediastinal mass, displacing the trachea in an anterolateral direction. Contrast esophagography revealed right lateral displacement of the cervical esophagus and superior mediastinum. Chest computed tomography (CT) was performed with contrast media, which showed the presence of a large mediastinal mass (12×14cm) with no contrast enhancement, located in the posterior visceral compartment, causing anterior displacement of the large vessels and trachea, and right anterolateral displacement of the esophagus (Fig. 1A).
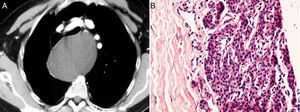
(A) The chest computed tomography with contrast medium shows a large mediastinal mass (12×14cm) without contrast enhancement causing anterior displacement of the large vessels and trachea, and anterolateral displacement of the esophagus. (B) Histopathological examination revealed a pseudocystic wall, which contained hypercellular parathyroid tissue (hematoxylin–eosin staining, original magnification 400×).
A possible clinical diagnosis of parathyroid cyst was established. Surgical resection was scheduled using a thoracotomic approach without preoperative fine needle aspiration of the cyst, in order to minimize the risk of mediastinitis and/or uncontrolled bleeding in the pleural space. The surgical strategy excluded video assisted thoracic surgery (VATS) due to the size of the cyst. We chose a classical posterolateral thoracotomy with muscle preservation, which allowed complete resection of the cyst with respect to the other mediastinal structures. Histopathological examination revealed a pseudocystic wall that included hypercellular parathyroid tissue (Fig. 1B).
The postoperative period was uneventful and the serum calcium concentration fell to 8.2mg/dl. The patient was discharged 5 days postoperatively.
On the contrast esophagography, carried out 3 months later, there was no displacement of the cervical and thoracic esophagus or stenosis. During the following 12 months, the serum calcium level remained within normal limits, so a cervical examination was not performed.
DiscussionMediastinal parathyroid cysts are relatively rare. These unusual lesions can present with locoregional clinical manifestations and, when they are active from a biochemical point of view, can also be associated with systemic symptoms. In 1925, de Quervain published the first case of satisfactory surgical resection of a parathyroid cyst in the mediastinal compartment,1 although to date fewer than 150 cases have been described among published studies.
The non-specific symptoms are related with the appearance of a space-occupying lesion, such as the one described in this report. The cysts can cause dyspnea as a result of marked tracheal deviation or stenosis, or dysphagia due to esophageal compression or deviation.
The differential diagnosis is usually established by radiological examinations combined with laboratory tests, which show an increase in the serum calcium and/or PTH concentration.
In the context of a state of hyperparathyroidism, a functioning mediastinal cyst must be considered, so its resection should be performed with simultaneous cervical examination, which is easy to perform for cervical cysts infiltrating or located in the anterior mediastinum. For parathyroid cysts in the posterior mediastinal compartment that require thoracotomy, simultaneous cervicotomy appears to be overtreatment, and should only be considered after demonstrating persistent hyperparathyroidism after surgery.
No deaths have been documented among published studies, although the resection of giant cysts can rarely be associated with postoperative complications.2 VATS has been described for the successful management of these cystic lesions, although all cases refer to small cysts located in the prevascular and anterior mediastinum.3–5
The exceptional nature of this report resides in the large size of the parathyroid cyst, which ruled out a VATS approach. However, it was successfully resolved using a thoracotomic approach without any postoperative morbidity, which resulted in complete clinical resolution of the presenting symptoms.
FundingThis study was carried out as part of research grant “Dottorato di Ricerca – XXVI ciclo – Scienze Chirurgiche – Alma Mater Studiorum Università degli Studi di Bologna”.
Please cite this article as: Davoli F, et al. Quiste paratiroideo funcionante gigante de localización mediastínica: una causa insólita de disnea de esfuerzo y disfagia de carácter leve. Arch Bronconeumol. 2013;49:408–9.