Computed tomography (CT)-guided radiofrequency ablation (RFA) is a minimally invasive technique used to treat solid tumors that offers a reliable alternative to surgery in oligometastatic lung disease1 and in early stage primary lung cancer.2 A major challenge in treating lung lesions with RFA has been the reliable evaluation of treatment response after the procedure. Unlike surgical resection, in which a histopathological analysis is performed post-procedure, the treated tumor is left in situ during RFA, so direct histopathological verification is not possible. The options currently available for post-procedure follow-up are CT,3 positron emission tomography (PET), and dual-modality imaging (PET-CT).4 CT and PET are unable to detect microscopic tumor foci and are less than optimal in the detection of early recurrence.5 Contrast-enhanced ultrasound (CEUS) is a technique that has been used for years in the immediate follow-up of the ablative treatment of focal lesions, especially in liver and kidney disease.6,7 Given the history of CEUS as a technique in evaluating the response of lesions treated with RFA in other parts of the anatomy, it is possible that in subpleural lesions accessible by ultrasound examination, CEUS may have the potential to be a complementary tool to CT and PET-CT in the evaluation of lung lesions treated by RFA.
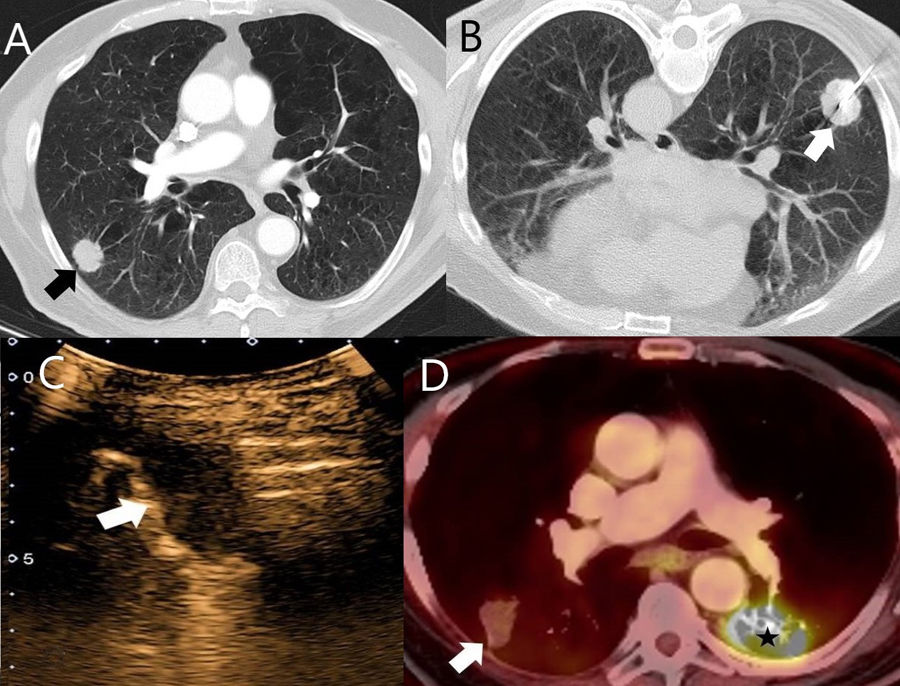
We present the case of a 73-year-old man who was diagnosed in August 2010 with cutaneous squamous cell carcinoma of the basal cells after years of skin lesions on the cheek and shoulder. Treatment involved surgical resection of the affected areas, and subsequent locoregional recurrences were also treated surgically. The patient then presented with a new recurrence involving 2 subpleural solid pulmonary nodules in the right lower lobe and another lesion in the left lower lobe. Palliative chemotherapy was administered, composed of carboplatin, 5-fluorouracil, and cetuximab, and complementary treatment with taxol. Subsequent radiological controls showed stable disease until November 2016, when an increase in the size of the lesions was reported (Fig. 1A). The multidisciplinary committee of our center decided to perform CT-guided RFA on the 2 lesions located in the right lower lobe and to apply radiation therapy to the contralateral lesion.
(A) Chest CT with iodinated IV contrast: lung window. A solid subpleural nodule (arrow) is seen in a patient with metastatic disease of cutaneous squamous cell carcinoma of the basal cells. This node was treated using CT-guided RFA. (B) Axial slice with patient in a supine position during CT-guided RFA. An umbrella needle (arrow) was used. (C) Pulmonary CEUS of the same lesion. No contrast uptake is observed throughout the procedure, indicating a complete response to ablative treatment. (D) Chest PET-CT of the same patient 1 year after ablative treatment, showing a decrease in the size of the treated lesion and no FDG uptake (arrow), consistent with a complete response. A pathological increase in FDG was observed in the left lower lobe lesion treated with radiation therapy (star).
On January 30th, 2017, CT-guided RFA was performed on the 2 nodules located in the right lower lobe. One lesion was treated with a 3cm umbrella needle (Fig. 1B), which resulted in mild pneumothorax and halo after treatment, and the other was treated with a 2cm straight needle. In the immediate follow-up CT, right pneumothorax was observed which required the placement of a chest tube, as the patient had developed dyspnea. He subsequently presented with moderate right pleural effusion, treated by ultrasound-guided pleural drainage on February 28th, 2017. During the procedure, pulmonary CEUS was performed to assess a potential infection in the lesion treated with RFA. The lesion showed no contrast uptake throughout the examination; this finding was suggestive of necrosis, indicating a complete response to RFA (Fig. 1C). Subsequent CT and PET-CT monitoring confirmed complete response to date (January 10th, 2019) (Fig. 1D).
CEUS has been shown to be a comparable alternative to CT and MRI in the evaluation of the response of neoplastic lesions treated with RFA, particularly in liver and kidney disease.6,7 In pulmonary CEUS, entities such as pulmonary infarctions or necrosis tend not to show contrast uptake during the entire examination,8 so in the post-RFA CEUS follow-up contrast enhancement would not be expected in lesions with complete response. Given the increasing use of RFA as alternative treatment to surgical resection in patients with oligometastatic or primary early-stage lung disease and the difficulty of detecting early recurrences by CT and PET-CT,5 pulmonary CEUS may be a complementary tool in the post-treatment monitoring of subpleural lesions accessible to ultrasound evaluation, especially when CT and PET-CT assessment are unclear. In addition, pulmonary CEUS may be useful to guide the biopsy of subpleural lesions in which recurrence is suspected.9
A factor limiting the evaluation of lung lesions by CEUS may be the lack of scientific literature available for the characterization of the different histological types of lung tumors, since only retrospective studies are available.10 As such, since the expected pretreatment appearance of lung lesions has not been established, it is difficult to compare them with the post-treatment image.
This is the first reported case of response assessment of percutaneous pulmonary treatment with CEUS. Additional studies are required to prove the usefulness of this technique in this context.
Please cite this article as: Páez-Carpio A, Vollmer I, Paredes P. Evaluación de la respuesta al tratamiento con radiofrecuencia de un nódulo pulmonar mediante ecografía con contraste (CEUS). Arch Bronconeumol. 2020;56:531–532.