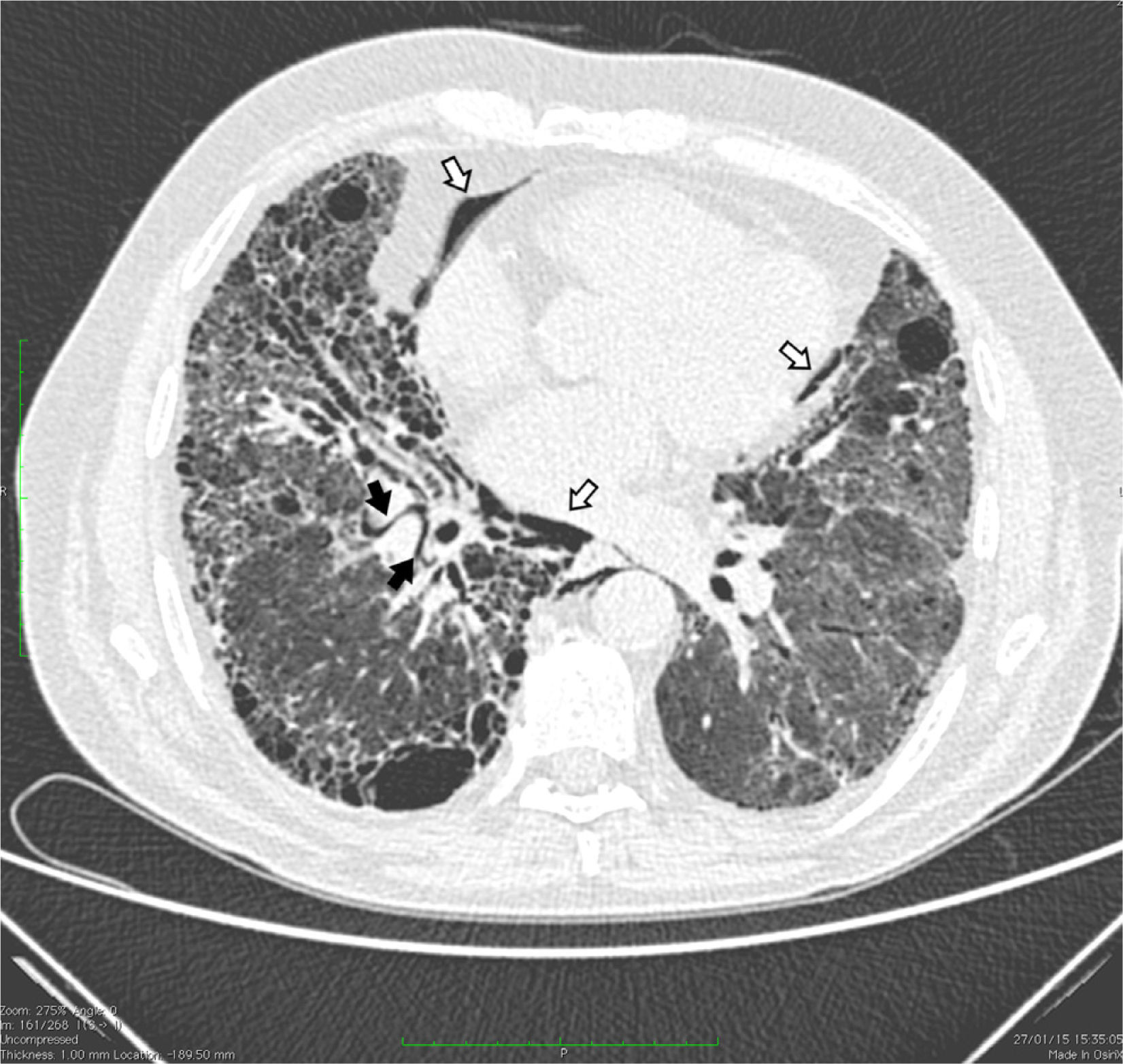
Interstitial emphysema (IE) is an uncommon lung disease associated with barotrauma, and is seen almost exclusively in neonates with respiratory distress syndrome. It is caused by the invasion of gas into the pulmonary interstitial space surrounding the bronchovascular bundles due to sudden changes in lung volumes and transpulmonary pressure. Secondary changes in the alveolar sacs cause the alveolar septa to rupture.1 The difference in pressure, always greater in the alveolar compartment than in the mediastinum, increases the flow of gas bubbles to the mediastinal compartment, producing pneumomediastinum. The effect of gravity causes the bubbles to rise to the neck, producing subcutaneous emphysema. We report the case of a 65-year-old man, former smoker (30 pack-years), with upper lobar emphysema and lower lobar fibrosis (combination of pulmonary fibrosis and emphysema [CPFE]). He presented in the hospital with worsening dyspnea at rest. On admission, he had intense tachypnea (32 breaths per minute) due to severe hypoxemia (38.5mmHg) and a heart rate of 90 beats per minute. Images from a high resolution computed tomography (HCRT) scan of the chest performed 1 year previously (not attached) showed significant involvement of the lung architecture with patterns of emphysema and concomitant fibrosis. Clinical diagnostic procedures were completed with full lung function tests (LFT) and spirometry. Approximately 4hours after spirometry, another chest HRCT was performed to compare the resulting morphological functional data with the previous examination. Unexpectedly, the repeat HRCT showed a significant amount of air in the mediastinal compartment (pneumomediastinum), and small gas bubbles were seen in the pulmonary interstitial space surrounding the bronchovascular bundles, attributed, in the absence of pneumothorax, to IE (Fig. 1). The patient had no signs of worsening chest pain or dyspnea after the HRCT or in the following hours. After 10 days of complete bed rest, another HRCT was performed, showing almost complete reabsorption of the air in the mediastinum and surrounding the bronchovascular bundles.
Chest computed tomography showing a thin curved line of gas surrounding the bronchovascular bundles of the right lower lobe, associated with interstitial emphysema (black arrows); extensive emphysematous changes were also observed in the mediastinum close to the heart and descending thoracic artery (pneumomediastinum: white arrows).
Episodes of this kind occurring after a routine spirometry are very rare, even in patients with a clinical history of CPFE. Apart from acute barotrauma in neonatal or pediatric patients, particularly in premature babies with respiratory distress syndrome treated with mechanical ventilation or patients with surfactant deficiency,2 few cases of IE have been described in the literature. This acute disease in adults is extremely rare: only occasional cases have been reported sporadically after lung transplant or in patients receiving high pressure continuous positive airway pressure ventilation, including a patient with severe pneumonia.3,4 In our patient, IE and pneumomediastinum were probably the result of alveolar rupture in the region of the bronchovascular bundles following the effort made on exhalation of air during spirometry. This may have produced a significant increase in thoracic pressure, causing over-distension of the alveoli and ductal/septal fracture. Extra-alveolar air moves in a centripetal direction around the mediastinum, and on some occasions, as in this case, can involve the soft tissues of the neck, producing subcutaneous emphysema.5 The patient received conservative treatment, with bed rest and close clinical monitoring. A few days later, the air had been completely reabsorbed, and the patient had recovered without complications.
Conflict of interestsThe authors state that they had no conflict of interests and receiving no funding for this article.
Please cite this article as: Rea G, Scotto di Frega G, Fiorentino G. Pulmonary interstitial emphysema following spirometry in CPFE syndrome. Arch Bronconeumol. 2015;51:602–603.