FOLFOX is the combination of 5-fluorouracil (5-FU), leucovorin (LV) and oxaliplatin. It is used in the treatment of colon cancer, both as a adjuvant therapy and in patients with metastasis.
Although lung toxicity has not been associated with either 5-FU or LV, several cases of interstitial pneumonia and organizing pneumonia have been reported with combinations containing oxaliplatin.1
We report the case of a patient with colon cancer who presented organizing pneumonia on completion of adjuvant treatment with FOLFOX.
A 73-year-old man with a diagnosis of stage IIC colon adenocarcinoma. After surgery, he received adjuvant FOLFOX. He completed 12 cycles that were well-tolerated with no clinical or radiological evidence of disease.
After completing the last treatment cycle, he presented in the emergency department with fever and cough with purulent expectoration. Physical examination showed: fever (38.7°C), tachypnea (21 breaths per minute), tachycardia (123 beats per minute), hypotension (90/50mmHg), basal oxygen saturation 92%, crackles in both lung bases, and regular heart rhythm, systolic ejection murmur heard at all areas. No evidence of septicemia or myelotoxicity on laboratory test results. Chest X-ray showing bilateral reticular interstitial infiltrates, predominantly in the left lung base. Electrocardiogram: sinus tachycardia; no other changes.
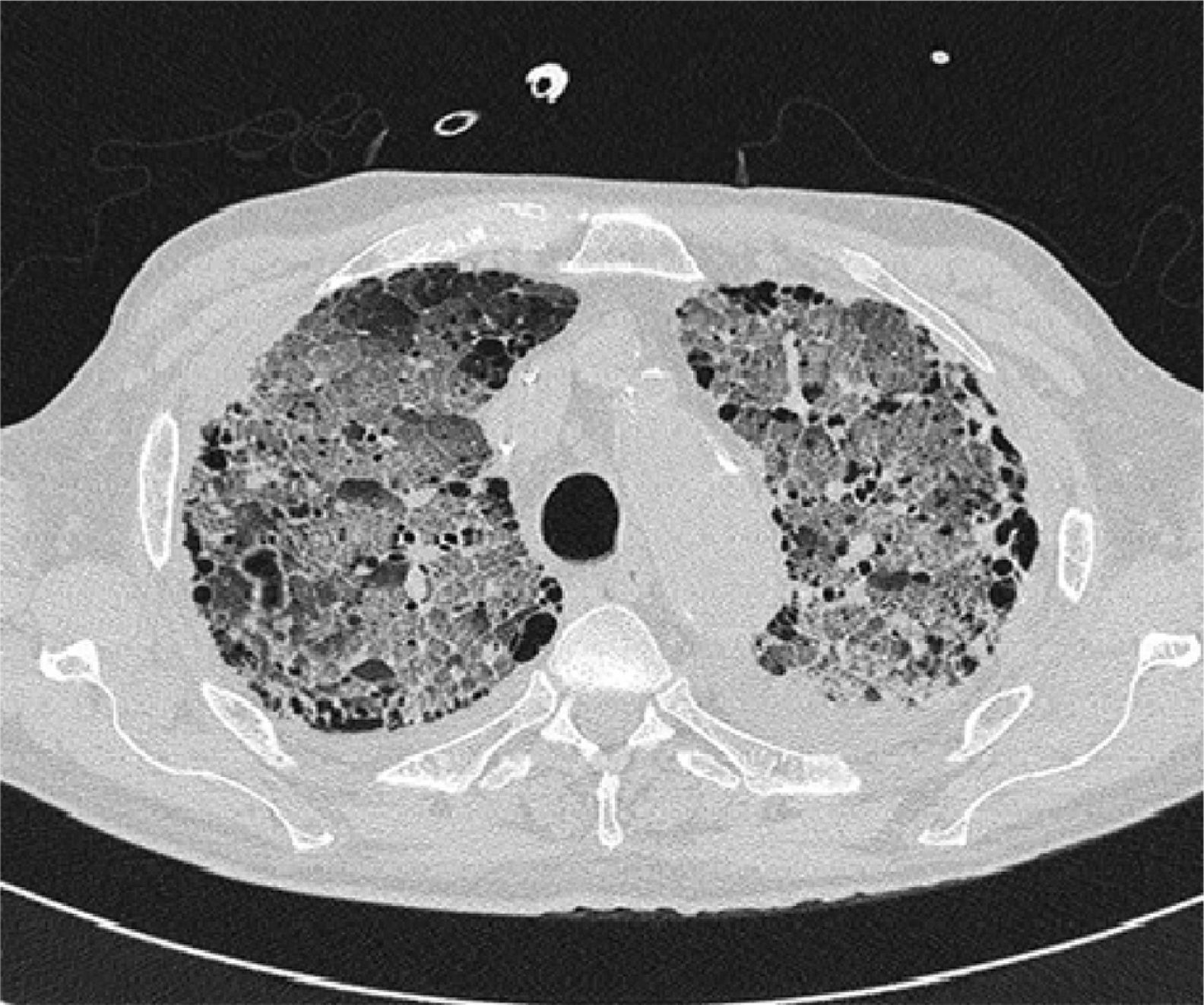
The guiding diagnosis was severe septicemia of respiratory origin, probably due to left basal pneumonia. Antibiotic treatment began with piperacillin/tazobactam and levofloxacin. The patient required admission to the intensive care unit for ventilatory and vasoactive support. Chest computed tomography (CT) showed signs of respiratory distress, but organizing pneumonia could not be ruled out (Fig. 1). Fiberoptic bronchoscopy did not reveal any macroscopic abnormalities, and no changes in cellularity were observed in bronchoalveolar lavage. Repeatedly negative cultures. H1N1 virus negative.
Differential diagnosis was given as either interstitial pneumonia or organizing pneumonia due to FOLFOX, so treatment with methylprednisolone 120mg/day was started, with an initially favorable response. When corticosteroid doses were reduced, the patient presented clinical and radiological deterioration, requiring mechanical ventilation with high FiO2 flows and high-dose vasoactive drugs. No improvement was observed, and the patient died.
On autopsy, significant pulmonary macroscopic involvement with a cobblestone effect and diffuse consolidation with no loss of overall architecture were observed. The microscopic examination showed extensive distortion of the pulmonary parenchyma, with different lesion patterns, the most significant of which were interstitial organizing pneumonia and areas of atypical alveolar epithelium, confirming the diagnosis of toxic organizing pneumonia caused by FOLFOX.
Pulmonary toxicity due to FOLFOX is uncommon and onset may be early or late.1,2 It has been suggested that oxaliplatin may be a causative agent, due to glutathione depletion in the alveolar epithelium. A similar phenomenon, affecting redox balance, is observed in liver tissue.3,4
Clinically, cough and dyspnea on exertion are the most common symptoms, while fever is infrequent.
The most common finding on chest CT include interstitial infiltrates and areas of ground glass opacity.1,2,4 Diffuse alveolar damage and organizing pneumonia are the most common histological findings, but histology data are rarely available.2,4 The recommended treatment consists of the administration of high-dose systemic corticosteroids, but even so, mortality is high.1,2,4
Please cite this article as: Vargas A, Montironi C, Buxó E. Neumonía organizada con desenlace fatal tras quimioterapia adyuvante con FOLFOX. Arch Bronconeumol. 2015;51:610.