Congenital lung and mediastinum malformations represent a wide and varied spectrum of development abnormalities, including cystic adenomatoid malformation (CAM), pulmonary sequestration, congenital lobar emphysema, bronchogenic cyst (BC), esophageal duplication cysts (EDC), and neurenteric cysts. These congenital malformations occur when the development of the respiratory system is altered. Differentiation begins after the third week of gestation, and 4 different stages have been defined: the embryonic phase, the pseudoglandular phase, the canalicular phase and the saccular phase. Altered development at any of these stages may cause bronchopulmonary malformations. Lung development is closely related with the development of the foregut, and for this reason these malformations commonly occur along with extrapulmonary congenital abnormalities. In the past, congenital bronchopulmonary anomalies were considered to be individual, distinct malformations, but nowadays more and more evidence is emerging to suggest that they share a similar etiopathological mechanism and overlapping clinical, radiological, and even histopathological features.1,2
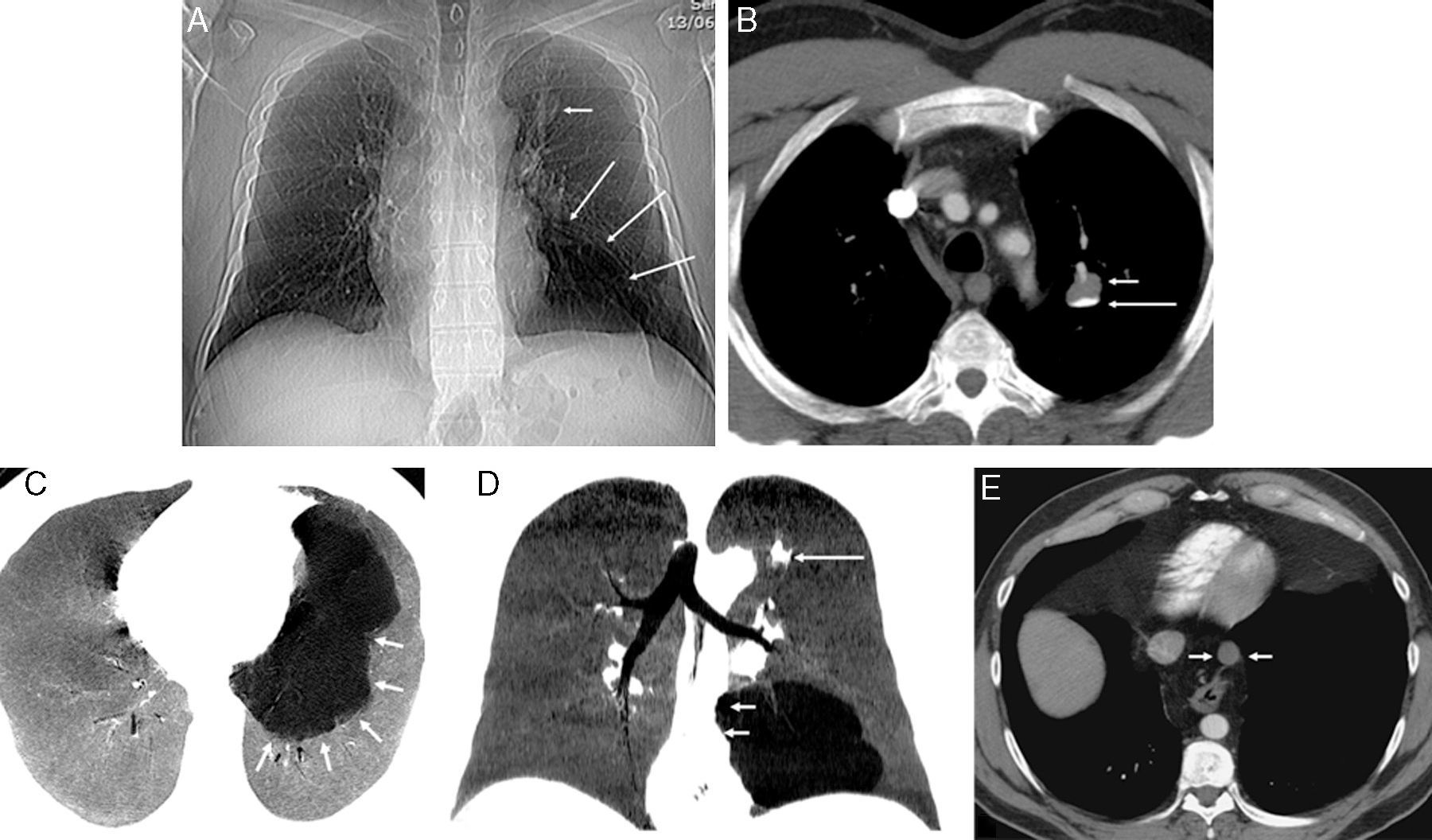
We report the case of a 43-year-old asymptomatic man with no significant clinical history. An incidental finding in a chest X-ray obtained before inguinal hernia surgery revealed a nodular lesion in the left upper lobe (LUL) and significant radiopacity in the left lung base (Fig. 1A). Chest computed tomography (CT) confirmed the existence of a cystic-type nodular lesion (no uptake of intravenous contrast medium) with well-defined margins in the LUL, showing characteristic fluid–fluid level. Supernatant fluid density was similar to water, while the sedimented fluid in the lower region of the nodular lesion had a calcific density (Fig. 1B). This typical sedimentation (supernatant with low attenuation and sediment with calcific density), called “milk of calcium”, is considered a pathognomic radiological sign of intrapulmonary BC,3 so we could confidently diagnose this entity. Moreover, a multicystic lesion suggestive of dysplasia/malformation, with no systemic vascularization and no apparent communication with the airway, was also observed in the basal segments of the left lower lobe. This lesion produced a mild mass effect on the adjacent lung parenchyma, shifting the mediastinum to the right side. Its radiological appearance was that of a type I CAM (Fig. 1C and D). Finally, in the lower posterior mediastinum, adjacent to the anterior esophageal wall, another single-cavity cystic lesion with well-defined margins was visualized. This lesion, which showed no uptake of intravenous contrast, had the appearance of an EDC (Fig. 1E). In the absence of thoracic symptoms, the patient decided to forego more aggressive diagnostic tests (except for an ultrasound-guided endoscopy for better characterization of the mediastinal lesion). He refused surgical intervention for the cystic lesions in the left lung.
(A) Chest X-ray showing nodular lesions in left upper lobe (LUL) (short arrow) and basal radiopacity with reduced blood perfusion (long arrows). (B) Axial computed tomography (CT) image of chest, confirming the presence of a cystic-type lesion in the left upper lobe, with typical fluid–fluid level. The supernatant (short arrow) has a density similar to water, while the density of the fluid in the lower part (long arrow) is calcific (calcium milk). (C) MinIP (minimum intensity axial projection) CT image showing a well-defined multicystic lesion (arrows), suggestive of malformation, in the left lower lobe basal segments, not communicating with the airway. (D) MiniIP coronal reconstruction showing a mild mass effect on the mediastinum towards the right side (short arrows). Note the nodular lesion in the LUL (long arrow). (E) Axial CT image showing a cystic lesion in the posterior mediastinum, adjacent to the anterior thoracic esophageal margin (arrows).
Incidental radiological findings of a development anomaly in the lungs or mediastinum of an adult are becoming more common, due to the more widespread use of multislice CT. When such findings are encountered, the radiologist is obliged to closely review the patient's images to rule out any other concomitant malformations which may have diagnostic or therapeutic implications.4,5 To the best of our knowledge, this is the first report in the scientific literature of 3 simultaneous congenital anomalies in the mediastinum and lung parenchyma (CB, CAM, and EDC).
Please cite this article as: Gorospe Sarasúa L, Ayala Carbonero AM, Fernández-Méndez MÁ. Asociación de tres anomalías del desarrollo pulmonar en un adulto. Arch Bronconeumol. 2016;52:113–114.